Ethical Concerns of AI in Surgery: A Homeopathic Approach
- Patient autonomy and informed consent challenges
- Accountability for AI decisions and errors
- Potential biases in AI algorithms affecting fairness
- Data privacy and security concerns with patient information
- Trust in AI’s decision-making transparency
- Resource allocation and its ethical implications
Artificial Intelligence (AI) has increasingly become integrated into healthcare, particularly in emergency surgery. While the potential of AI to improve decision-making and patient outcomes is evident, its use raises critical ethical questions. Addressing these concerns is essential to ensure patient safety, preserve medical integrity, and maintain trust in healthcare systems.
Autonomy vs. AI Decision-Making
AI systems in emergency surgery are designed to assist or even autonomously make clinical decisions. However, this raises the issue of patient autonomy. Traditionally, patients have the right to make informed decisions regarding their treatment. When AI plays a dominant role in these decisions, the extent to which patient consent is respected becomes a challenge.
Key ethical concerns:
- Is the patient aware of AI’s involvement in their care?
- How much control does the patient retain over the final decision?
- Are healthcare professionals transparently communicating AI’s role?
In high-pressure situations like emergency surgeries, patients often cannot give full consent. In such scenarios, AI might make critical decisions. The question remains—should AI have the ultimate say, or should the final decision rest with a human professional, even if AI’s recommendation is statistically superior?
Accountability and Liability
In traditional medical practice, if a surgical error occurs, the surgeon or medical team is held accountable. The introduction of AI complicates this scenario. If AI misjudges a situation or a system failure results in harm, who bears the responsibility?
Areas of concern:
- If AI provides incorrect recommendations, can the healthcare provider be blamed for following the advice?
- If the healthcare provider overrides AI’s suggestion and the outcome is negative, does liability shift back to the human professional?
- Who is legally accountable: the healthcare institution, the AI developers, or the regulatory bodies?
Healthcare professionals may find themselves in a conflicted position between trusting AI’s data-driven accuracy and relying on their personal clinical experience.
Bias in AI Algorithms
AI systems are trained on historical data. This data may reflect societal biases or limitations in the diversity of the populations it represents. Bias in AI can manifest in emergency surgery by providing unequal outcomes for different demographic groups, particularly racial minorities or those with atypical medical histories.
Ethical questions to consider:
- How can we ensure AI algorithms are free from bias?
- What measures are in place to continuously update and refine AI systems?
- How transparent are the algorithms in terms of the data they use for decision-making?
Bias mitigation must be a priority in the design and implementation of AI systems, particularly when they are used in life-or-death situations.
Data Privacy and Security
AI in emergency surgery relies on vast amounts of patient data to make accurate and timely decisions. This reliance on data brings privacy concerns to the forefront, especially when sensitive patient information is involved.
Challenges:
- Ensuring that the collection and use of data complies with data protection regulations.
- Avoiding the misuse of data, especially if it is shared with third-party developers.
- Guaranteeing that patient data is anonymized where possible to prevent identity breaches.
In emergencies, when time is of the essence, ensuring robust data security protocols may be difficult, increasing the potential for data vulnerability.
Informed Consent in AI-Driven Emergencies
The use of AI in emergency surgery often bypasses the traditional informed consent process. In an emergency, patients may not have the time or capacity to give full consent, and when AI is involved, they may be less informed about the extent of its role in their care.
Ethical dilemmas:
- Should patients be informed that AI will be used in their surgery, even in emergencies?
- Can AI be ethically deployed without patient knowledge if it’s deemed to improve outcomes?
- How can informed consent procedures be adapted to include AI in emergency settings?
Ensuring that patients are as informed as possible, even in constrained timeframes, is vital for maintaining trust in healthcare systems.
Transparency and Trust in AI Systems
Transparency is critical in fostering trust between healthcare professionals and patients when AI is used. Black-box algorithms—where the decision-making process of AI is not easily understood—create mistrust and hinder accountability.
Crucial points for transparency:
- Providing clear explanations of how AI makes decisions.
- Regular audits of AI systems to ensure reliability and fairness.
- Offering healthcare providers easy-to-understand reports on how AI reached its conclusions.
Without transparency, even the most accurate AI system may face resistance from both patients and practitioners.
Resource Allocation and Fairness
AI can optimize resource allocation in emergency surgery, ensuring that critical supplies, personnel, and equipment are used efficiently. However, its role in resource prioritization raises ethical questions about fairness, particularly in under-resourced environments.
Considerations:
- Does AI prioritize patients based solely on medical need, or are economic factors also considered?
- Is there a risk that marginalized populations receive lower priority based on algorithmic predictions?
AI systems must be designed to allocate resources fairly, without exacerbating existing inequalities in healthcare access.
Surgeon’s Role in the Age of AI
With AI taking a more prominent role in emergency surgeries, the role of the surgeon may shift. Surgeons may transition from decision-makers to overseers who verify AI’s recommendations. This change could impact the professional satisfaction and mental well-being of surgeons.
Key challenges:
- How does AI integration affect the surgeon’s role in patient care?
- What ethical responsibility does the surgeon retain if AI is the primary decision-maker?
- Will surgeons receive adequate training to supervise AI systems effectively?
Ensuring that AI complements rather than replaces human skills is essential to maintaining a balanced surgeon-patient relationship.
Ethical AI Development and Oversight
AI developers and healthcare institutions share a responsibility to ensure that AI systems are ethically designed and implemented. Continuous oversight from regulatory bodies, ethical committees, and independent audits is necessary to ensure AI systems meet safety and ethical standards.
Critical measures:
- Regularly testing AI systems for bias and inaccuracies.
- Updating AI algorithms to reflect current medical knowledge and ethical standards.
- Ensuring human oversight remains a key component in the deployment of AI.
By establishing clear ethical guidelines and regulatory frameworks, the healthcare industry can ensure that AI in emergency surgery is both effective and ethical.
Balancing Innovation with Ethics
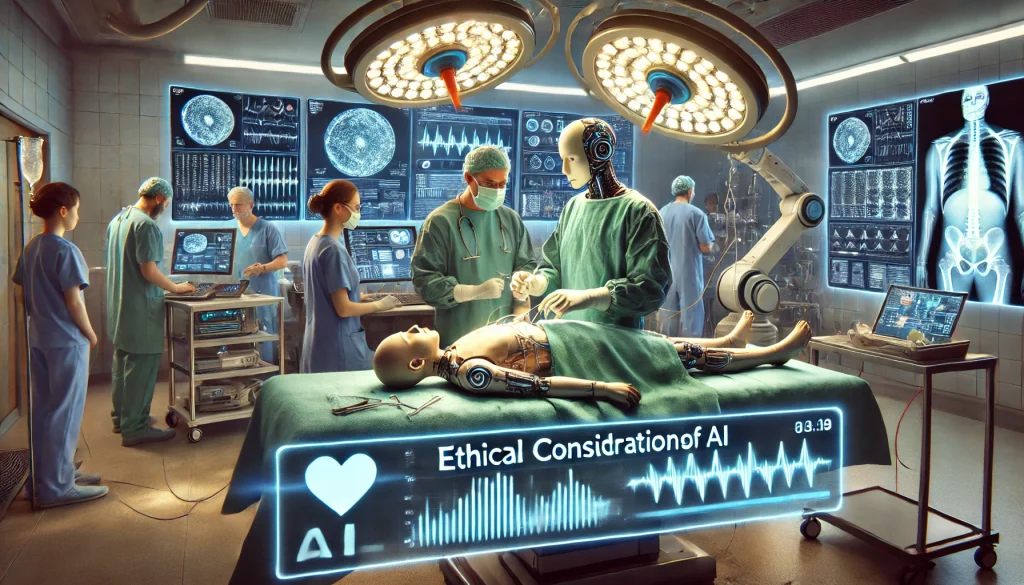
The use of AI in emergency surgery is transformative, but it brings numerous ethical challenges. While AI has the potential to save lives, it also risks compromising patient autonomy, privacy, and fairness. Striking a balance between technological innovation and ethical responsibility is crucial for the future of healthcare.
Maintaining transparency, ensuring fair resource allocation, and preserving accountability are essential to the ethical use of AI in emergency settings. Both healthcare professionals and AI developers must work together to ensure that AI systems benefit all patients while respecting core medical ethics.
Top 10 Real-Life Use Cases: Ethical Considerations of AI in Emergency Surgery
1. Patient Autonomy in Decision-Making
AI can assist in decision-making, but the balance between AI-driven suggestions and patient autonomy needs attention. In emergency situations, patients might not have time for informed consent, raising concerns about the extent to which they control their treatment.
2. AI Accountability and Liability
Determining who is accountable when AI leads to poor outcomes is complex. Healthcare providers must balance reliance on AI while maintaining responsibility for decisions made during surgery, especially when outcomes are negative.
3. Bias in AI Algorithms
AI systems trained on biased data may unintentionally offer suboptimal treatments for certain populations, especially underrepresented groups. Continuous refinement of AI algorithms is necessary to avoid discrimination in treatment recommendations.
4. Data Privacy and Security
AI relies on vast amounts of patient data, raising concerns about data security and privacy. Emergency situations may require quick data access, which must be balanced with patient confidentiality and legal requirements, such as GDPR.
5. Transparency and Trust in AI Decisions
AI often operates as a “black box,” meaning its decision-making process is not transparent. Surgeons need to understand AI recommendations clearly, fostering trust in AI-driven surgery and ensuring they can explain the decisions made.
6. Real-Time Data Accuracy
In emergency surgery, the quality of real-time data is critical. Faulty or outdated data can result in inaccurate recommendations from AI, compromising patient safety. Ensuring high-quality, real-time data is one of the significant challenges.
7. Ethical Concerns of AI Resource Allocation
AI is often used to optimize resource allocation during emergencies. However, there are concerns that it might prioritize patients based on biased criteria, such as socioeconomic status, rather than strictly medical need.
8. Surgeon’s Role with AI Assistance
AI is intended to assist, not replace, surgeons. However, over-reliance on AI may reduce the surgeon’s active involvement, potentially diminishing their role in critical decisions. Balancing AI assistance with human expertise is key to ethical practice.
9. Informed Consent in AI-Driven Surgery
Informed consent becomes more challenging when AI is involved. Patients should know how AI is used in their treatment, but in emergencies, obtaining detailed consent might not be feasible, raising ethical questions about patient rights.
10. Legal and Ethical Oversight
The use of AI in surgery requires robust regulatory frameworks to ensure ethical standards are met. Ongoing oversight, regular audits, and ethical reviews help ensure that AI operates within safe, transparent, and fair guidelines.
Frequently Asked Questions: Ethical Considerations of AI in Emergency Surgery
What ethical concerns arise with AI making surgical decisions?
The main concerns involve patient autonomy, transparency in AI decision-making, and accountability in case of errors or negative outcomes.
Who is responsible if AI makes a wrong decision during surgery?
Accountability is shared between the healthcare provider, AI developers, and possibly the healthcare institution, depending on the situation.
How can AI respect patient autonomy during emergencies?
Balancing quick AI decisions with patient consent is difficult, especially in emergencies where consent may not be fully possible. Ensuring informed consent when possible is crucial.
Does AI discriminate in emergency surgical decisions?
AI can show bias if trained on biased data. Ensuring fairness in AI requires continuous refinement and regular updates to prevent unequal treatment.
Can AI explain its decisions in real-time surgeries?
AI often works as a “black box,” meaning it cannot always explain how decisions are made. Ensuring transparency in AI decision-making is critical for building trust.
What role does data privacy play in AI-driven surgery?
AI uses vast amounts of patient data to make decisions, raising concerns about how securely this data is stored and accessed, especially in emergencies.
Is AI faster than human surgeons in making decisions?
AI processes data quickly, providing real-time recommendations, but its ability to work in sync with human expertise is key to effective use.
How does AI impact the role of surgeons in emergency settings?
AI assists surgeons by providing recommendations, but surgeons still make the final decisions. Over-reliance on AI may reduce their active participation.
Can AI help allocate resources fairly during emergencies?
AI optimizes resource use but may unintentionally prioritize patients based on biased factors. Ensuring fairness in resource allocation is a critical concern.
What is the biggest challenge for AI in emergency surgery?
The main challenge is ensuring real-time data accuracy while making decisions that respect patient rights and ethical standards in high-pressure situations.
How does AI handle complex ethical decisions in emergencies?
AI lacks emotional intelligence and ethical reasoning, which are crucial in life-and-death situations. Combining AI’s speed with human judgment is necessary.
Can patients refuse AI-driven treatments?
Patients should have the right to know if AI is involved and can refuse AI-driven treatment, though this is harder to navigate in urgent emergencies.
What legal regulations exist for AI in surgery?
Laws and guidelines are still evolving, but ensuring accountability, patient safety, and data privacy are at the core of most regulations.
How do surgeons ensure AI’s recommendations are correct?
Surgeons must be trained to interpret AI outputs critically and use their own clinical judgment to make final decisions.
Can AI reduce errors in emergency surgery?
AI can help reduce errors by providing data-driven recommendations, but its effectiveness depends on the quality of data and the expertise of the surgeons using it.