Overcoming Key Challenges in AI Emergency Surgery Settings
- Ensuring data accuracy and reliability during critical operations
- Balancing patient privacy with AI’s need for extensive data
- Integrating AI recommendations with surgeon expertise
- Addressing bias in AI algorithms that affect treatment outcomes
- Managing real-time decision-making without compromising safety
- Establishing clear accountability in case of AI errors
Data Accuracy and Reliability
AI in emergency surgery depends on real-time data to make critical decisions. However, challenges arise when this data is inaccurate or incomplete. Surgeons must trust AI’s recommendations, but faulty inputs can lead to dangerous consequences. Real-world data from patients, including their medical history and current status, might not always be available in a format that AI systems can efficiently process, leading to potential errors.
Patient Privacy Concerns
Emergency settings often require rapid decisions, which means AI must access a vast amount of patient data quickly. Maintaining patient privacy while ensuring AI systems have enough information to operate effectively poses a significant challenge. Encryption methods, data anonymization, and compliance with privacy laws like GDPR are essential to ensuring data integrity and patient trust. However, balancing these legal requirements with the speed needed in emergencies can be difficult.
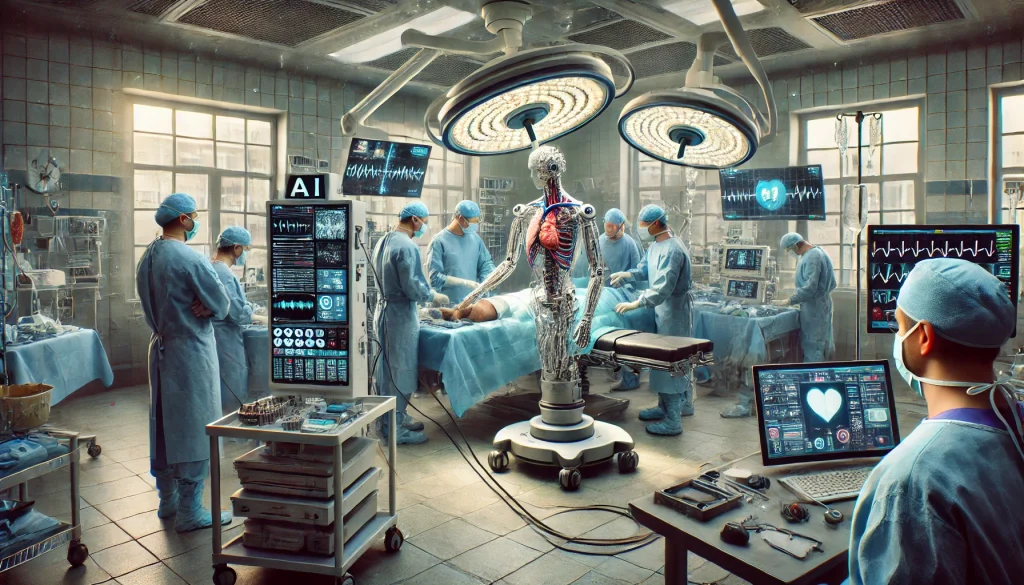
Integration with Human Surgeons
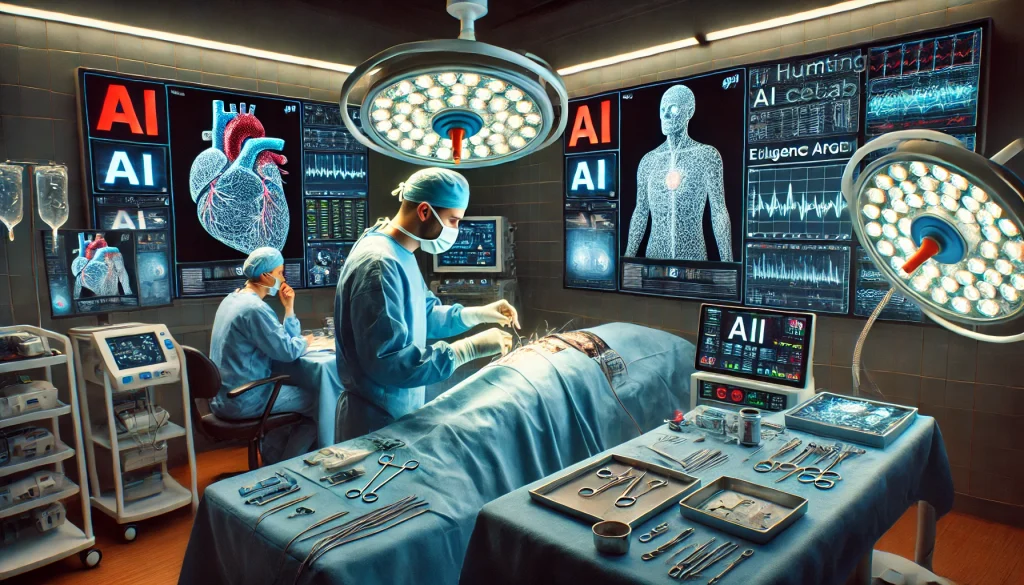
The role of AI in emergency surgery is not to replace surgeons but to assist them. Yet, integrating AI decision-making with the expertise of human professionals can lead to conflict or hesitation. Surgeons may question whether to trust AI recommendations over their own experience, particularly in high-stakes situations. Ensuring a seamless collaboration between human judgment and AI suggestions remains one of the most pressing challenges.
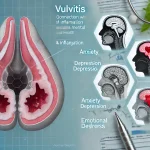
Bias in AI Algorithms
Bias within AI algorithms poses risks in emergency surgery. The algorithms are often trained on historical data, which can include biases against specific populations or underrepresented groups. As a result, AI systems may disproportionately affect minority patients by offering suboptimal or even harmful recommendations. This makes it imperative to continuously monitor and correct biases in AI training data to prevent discrimination and ensure fair treatment for all patients.
Real-Time Decision Making Under Pressure
One of AI’s promises is its ability to quickly process large datasets and make informed decisions. However, the pressure of real-time decision-making in emergency situations introduces new risks. AI systems must operate swiftly but without sacrificing accuracy, and surgeons must be able to trust that AI will not delay or misinterpret data during critical moments. Managing this balance between speed and safety is a significant challenge.
Ethical Accountability and Liability
Who is responsible when AI systems make mistakes? If AI suggests an incorrect course of action that leads to a negative outcome, determining liability can be complex. Should it be the surgeon who followed the AI’s guidance, the healthcare institution, or the developers of the AI system? The lack of clarity on accountability is one of the core ethical challenges surrounding AI use in emergency surgery.
Cost and Accessibility
AI technology requires significant financial investment. This leads to disparities in access, where wealthier hospitals may benefit from advanced AI tools while underfunded facilities lag behind. Consequently, patients in certain regions may not benefit from the most cutting-edge AI advancements, leading to uneven healthcare outcomes globally. The cost and scalability of implementing AI in all healthcare facilities is a pressing issue.
AI Interpretability and Transparency
Many AI systems, particularly those based on deep learning, are considered “black boxes.” This means that while they produce results, the process by which they arrive at their recommendations is not always transparent. Surgeons and healthcare professionals may find it difficult to trust AI systems if they cannot fully understand or explain how a decision was made. Ensuring AI transparency is key to gaining trust and improving collaboration between surgeons and machines.
Training and Education
The introduction of AI into emergency surgery requires extensive training for healthcare professionals. Surgeons and medical staff need to be proficient not only in using AI systems but also in understanding their limitations. Developing comprehensive education programs that teach medical professionals how to collaborate with AI, recognize its shortcomings, and incorporate it into their practices is crucial for its success.
Legal and Regulatory Frameworks
Governments and regulatory bodies must establish clear guidelines for the use of AI in emergency surgeries. This includes ensuring ethical standards, patient safety, and accountability measures are strictly followed. Regulatory delays or lack of cohesive policies can slow down AI adoption and lead to confusion about its proper use in high-risk environments. Comprehensive legal frameworks must be developed and updated to keep pace with technological advancements in AI.
Top 10 Real-Life Use Cases of Challenges in AI Emergency Surgery
1. Data Collection and Quality Control
In emergency surgery, accurate data is critical. AI systems may struggle with incomplete or inaccurate patient data, affecting the quality of recommendations. Effective data management ensures the reliability of the AI system’s output, but errors may lead to poor decision-making.
2. Surgeon-AI Collaboration
AI assists surgeons in emergencies by providing rapid analysis. However, trust between AI systems and surgeons is crucial. Surgeons may hesitate to follow AI suggestions, especially when outcomes are uncertain. Building trust between the two is key to successful implementation.
3. Algorithm Bias
AI systems may inadvertently learn biases from historical data. In emergency settings, this can lead to unfair treatment decisions, particularly in underrepresented patient populations. Addressing biases ensures that AI recommendations are equitable and reliable.
4. Ethical and Legal Accountability
In cases where AI recommendations lead to adverse outcomes, liability issues arise. It’s unclear whether the AI developers, medical staff, or the healthcare institution hold responsibility. Clear legal frameworks need to address these complexities to protect both patients and healthcare providers.
5. Real-Time Data Processing
AI in emergency surgery requires fast and accurate data processing. Delays in processing can have catastrophic consequences. Optimizing AI systems to handle vast amounts of real-time data while maintaining precision remains a challenge for developers and healthcare providers.
6. Patient Privacy and Data Security
AI systems in emergency surgery handle sensitive patient information. The challenge is to balance data privacy with the need for real-time access to critical patient data. Secure data handling practices are essential to prevent breaches while providing timely insights.
7. Complexity of Multi-Disciplinary Data
Emergency surgeries often require input from multiple departments, creating a complex web of data for AI to process. Integrating various medical data in real-time for accurate AI predictions is a significant technical challenge, requiring advanced algorithms and hardware.
8. Surgeon Training and Education
Surgeons need to understand how AI works to use it effectively in emergencies. Training programs must be developed to teach surgeons how to interpret AI outputs and make informed decisions without over-reliance on technology.
9. Bias in Treatment Recommendations
When AI suggests treatments, it may favor particular approaches based on biased training data. This could lead to the overuse of certain procedures, creating a treatment gap. Reducing such biases ensures all patients receive the most appropriate care.
10. Ethical Decision-Making in AI
AI lacks the emotional intelligence required for complex ethical decisions in emergencies. When decisions involve life and death, AI cannot consider personal or moral values. Combining human empathy with AI’s data-driven accuracy is crucial to making balanced decisions.
Frequently Asked Questions on Challenges in AI Emergency Surgery
What are the main challenges AI faces in emergency surgery?
Data reliability, algorithm bias, and ensuring surgeon-AI collaboration are some of the key challenges in AI’s effective use in emergency surgery.
How does AI affect surgeon decision-making in emergencies?
AI provides real-time analysis, but surgeons must weigh these suggestions against their own expertise. Trust and collaboration are essential.
Is AI fully reliable in making emergency surgical decisions?
AI’s reliability depends heavily on the quality of the data it receives. Inaccurate or incomplete data can lead to mistakes in recommendations.
Can AI be biased in emergency surgery?
Yes, AI systems can reflect biases from the data they were trained on, leading to unfair treatment recommendations in some cases.
Who is responsible if AI makes a mistake in surgery?
Accountability remains a gray area. There is ongoing debate about whether the responsibility lies with the surgeon, the institution, or the AI developers.
How can surgeons be sure that AI recommendations are accurate?
Surgeons must be trained to critically evaluate AI suggestions and always verify the AI’s output with their own clinical judgment.
Can AI handle the pressure of real-time decision-making in emergencies?
AI is capable of rapid analysis, but ensuring that it processes large amounts of data accurately without delay is still a challenge.
What role does data privacy play in AI emergency surgery?
Protecting sensitive patient information while allowing AI to access real-time data quickly is a significant concern, especially in high-pressure situations.
How can bias in AI algorithms be mitigated in emergency settings?
Regular monitoring and updates of the AI’s training data are required to ensure it is free from bias and provides equitable treatment options.
Does AI replace human surgeons in emergency procedures?
No, AI assists surgeons but cannot replace the human judgment, expertise, and empathy required in emergency settings.
What legal frameworks are in place for AI use in surgery?
Legal frameworks are still evolving, with ongoing discussions about setting clear guidelines for the ethical use and accountability of AI in surgical environments.
How do surgeons and AI collaborate in real-time surgery?
AI assists by providing rapid data analysis, but surgeons must still make the final decisions based on a combination of AI inputs and their own clinical expertise.
Can AI improve patient outcomes in emergency surgery?
AI has the potential to improve outcomes by providing real-time insights, but its effectiveness depends on data quality, bias management, and surgeon collaboration.
Is AI training for surgeons necessary?
Yes, surgeons need to be trained on how to interpret AI outputs and effectively integrate AI systems into their practice, especially in fast-paced emergency environments.
What are the ethical concerns of using AI in life-or-death situations?
Ethical concerns include decision-making transparency, accountability, data privacy, and ensuring that AI recommendations do not compromise patient rights or safety.