Advancing Orthopedic Surgery with AI and Predictive Analytics
- Improved Diagnosis: AI-driven imaging helps detect conditions early, aiding accurate diagnosis.
- Risk Assessment: Predictive analytics identify patient-specific surgical risks.
- Personalized Treatment: AI customizes treatment plans based on unique patient data.
- Optimized Recovery: Predictive models enhance postoperative care and recovery timelines.
- Enhanced Operating Room Management: AI improves scheduling and workflow.
Orthopedic surgery is evolving rapidly, with advanced technologies reshaping how we approach patient care and outcomes. Artificial intelligence (AI) and predictive analytics have emerged as powerful tools in this field, providing data-driven insights that enhance diagnosis, treatment planning, and postoperative recovery. By integrating AI into orthopedic care, surgeons can make more informed decisions, predict complications, and even optimize recovery plans, all leading to better overall outcomes for patients. Here, we’ll explore how AI and predictive analytics are redefining orthopedic surgery and improving lives through precision, efficiency, and personalized care.
The Role of AI in Orthopedic Surgery: A New Era of Precision
Orthopedic surgery involves intricate procedures on bones, joints, and ligaments, often requiring a high level of precision and planning. AI in orthopedics addresses these complexities by analyzing large datasets from past surgeries, patient records, imaging studies, and more. By processing this data, AI identifies patterns that human eyes may miss, predicting potential outcomes and risks with impressive accuracy.
For instance, in total knee and hip replacements, AI can analyze past surgical data to help surgeons choose the most appropriate implant type, alignment, and positioning for a specific patient. This precision significantly reduces postoperative issues, such as joint instability or wear. Moreover, AI can help surgeons simulate surgery, allowing them to plan each step before even making the first incision. This preoperative visualization has proven invaluable, as it enables surgeons to anticipate and address challenges in advance.
Predictive Analytics in Orthopedic Surgery – Anticipating Risks and Outcomes
Predictive analytics in orthopedics focuses on assessing risk factors and predicting patient-specific outcomes based on available data. With tools that analyze a wide range of patient information—from genetic predispositions to lifestyle factors—predictive analytics provides a clearer picture of each patient’s unique surgical risks.
Let’s take spinal fusion surgery as an example. It’s a complex procedure with a risk of complications, such as non-union (where the bones fail to fuse properly) or infection. Predictive analytics uses data from thousands of cases to calculate the likelihood of these complications, which helps surgeons develop tailored pre- and postoperative plans to minimize risks. These insights enable healthcare providers to adjust surgical approaches or implement preventive measures, all while keeping the patient’s unique profile in mind.
Enhancing Diagnosis Through AI-Powered Imaging
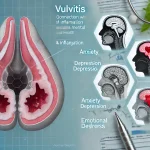
One of the most transformative uses of AI in orthopedic surgery is in medical imaging and diagnostics. Traditional imaging technologies like X-rays, MRIs, and CT scans are essential in identifying issues such as fractures, ligament tears, and arthritis. However, interpreting these images accurately can sometimes be challenging due to subtle differences between normal and abnormal tissue.
AI-powered diagnostic tools can analyze imaging data far beyond what the human eye can detect, recognizing subtle patterns that indicate early signs of disease. For example, in patients with osteoarthritis, AI can identify degenerative changes in cartilage at a much earlier stage, allowing for timely intervention. By catching conditions early, AI-supported diagnostics help prevent disease progression and, ultimately, reduce the need for invasive surgeries.
Personalizing Patient Care – AI-Driven Treatment Plans
In orthopedics, treatment needs vary widely between patients, even if they present with similar conditions. AI-driven personalized treatment plans consider a patient’s unique medical history, lifestyle, and recovery goals, allowing for truly tailored care. This approach is especially valuable in complex cases such as rotator cuff repairs or ACL reconstructions, where patient-specific factors can influence recovery speed and success.
With AI, surgeons can recommend treatment plans based on data from similar patient profiles, including expected recovery timelines, optimal physical therapy routines, and even specific surgical techniques that have shown success in patients with similar backgrounds. This customized approach improves outcomes by ensuring that every step of the patient’s journey—from pre-surgery preparation to recovery—is optimized for their individual needs.
Improving Postoperative Recovery Through Predictive Models
Recovery can vary greatly in orthopedic surgery, with factors like age, physical condition, and previous injuries playing a role in healing. Predictive models use data from large patient populations to forecast recovery timelines, identifying patients who may require additional support to reach full function.
For example, following a knee replacement surgery, predictive analytics can estimate the patient’s range of motion at different stages of recovery. If the model predicts slower progress, the healthcare team can proactively adjust the physical therapy plan or incorporate additional interventions to help the patient regain movement. This data-driven approach enables a more responsive recovery process, reducing the likelihood of setbacks and improving the patient’s overall quality of life.
Reducing Surgical Complications and Readmissions
Preventing complications and minimizing readmissions are key priorities in orthopedic care. AI and predictive analytics help healthcare providers manage both by analyzing risk factors that may increase the chances of complications, such as blood clots, infections, or delayed healing.
Take hip fractures in older adults, which often carry a high risk of complications due to age-related factors. Predictive models can highlight patients at higher risk for post-surgical complications, enabling the healthcare team to monitor these patients closely and adjust treatment as needed. Additionally, AI tools can assist in creating personalized follow-up schedules, ensuring timely check-ins and reducing the likelihood of emergency readmissions.
Optimizing Operating Room Performance with AI
In a busy orthopedic department, efficient use of operating room (OR) time is critical for ensuring patients receive timely care. AI has proven useful in scheduling and workflow management, analyzing data to predict the duration of surgeries and helping staff allocate resources effectively.
AI algorithms assess factors like the complexity of the procedure, surgeon experience, and patient-specific needs, estimating how long each surgery will take. This helps hospitals optimize OR schedules, reduce wait times, and increase the number of patients who can be treated each day, making orthopedic care more accessible without compromising quality.
Improving Pain Management and Postoperative Care
Managing pain effectively after orthopedic surgery is crucial for successful recovery. AI-driven pain management systems can track patient-reported pain levels and analyze patterns to predict when a patient might experience peak pain or discomfort. This allows doctors to prescribe the most effective pain relief methods and dosage schedules, preventing under-treatment or overuse of medication.
AI also assists in identifying patients who may benefit from alternative pain management options, such as physical therapy, nerve blocks, or non-opioid medications. By predicting pain patterns, healthcare providers can proactively address patient needs, making the recovery process more comfortable and reducing reliance on opioid-based pain relief.
Advancing Robotic Surgery in Orthopedics
AI has played a pivotal role in robot-assisted surgeries, where precision is paramount. In procedures like knee or hip replacements, robotic systems guided by AI algorithms allow for exact incisions and placements that reduce tissue damage and promote quicker healing.
These robotic systems can perform tasks with millimeter-level precision, allowing surgeons to avoid surrounding muscles and nerves, leading to faster recovery times and reduced post-surgery pain. The combination of human expertise with AI’s computational power enables a level of accuracy that would be difficult to achieve manually, ultimately improving patient outcomes and satisfaction.
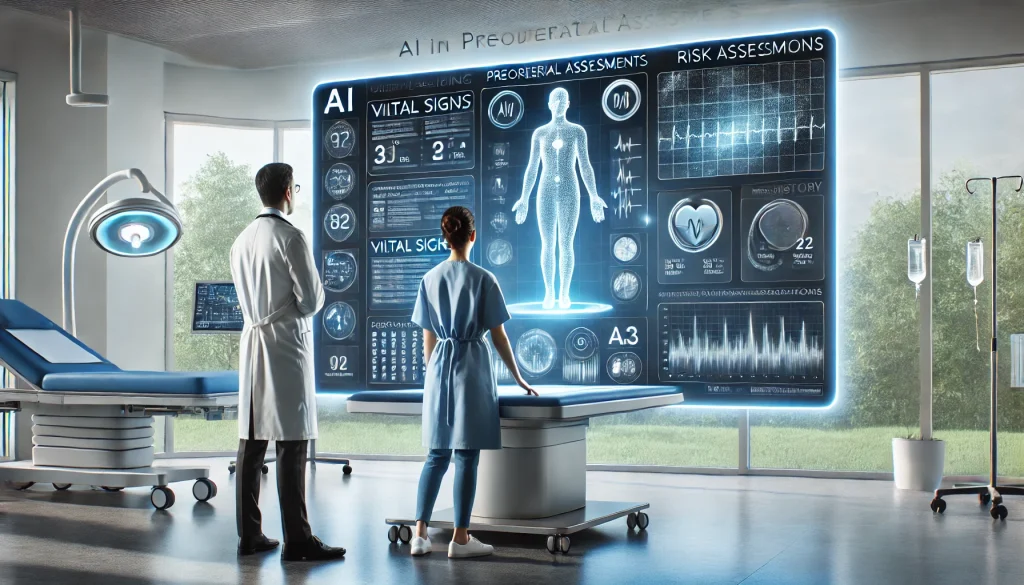
Streamlining Preoperative Assessments with AI
Before undergoing orthopedic surgery, patients typically require a series of assessments to ensure they are healthy enough for the procedure. AI-driven assessment tools can evaluate a patient’s medical history, lab results, and lifestyle factors to determine their surgical readiness. This approach not only makes preoperative evaluations faster but also more accurate, ensuring that high-risk patients are identified early and provided with additional care.
For patients with pre-existing conditions such as diabetes or cardiovascular disease, AI tools can recommend additional pre-surgical preparations, minimizing risks associated with surgery. By refining the preoperative process, AI helps make surgeries safer and improves patient confidence in their surgical team.
Enhancing Patient Education and Engagement
Finally, AI-powered educational tools are transforming patient engagement in orthopedic surgery. These systems provide personalized educational content, explaining the surgical process, potential risks, and recovery milestones, empowering patients to make informed decisions about their care.
AI-based applications can guide patients through preoperative exercises, post-surgery rehabilitation routines, and lifestyle adjustments, offering reminders and progress tracking. This level of engagement helps patients stay informed, adhere to their recovery plans, and feel more confident about their healing journey. The ability to understand and participate actively in one’s care is a significant factor in achieving better outcomes and lasting improvements.
Looking Ahead – The Future of AI in Orthopedic Surgery
The integration of AI and predictive analytics into orthopedic surgery is an exciting development that holds immense potential. As AI technologies continue to evolve, we can expect even greater precision, more personalized care, and shorter recovery times for patients. By improving every stage of the orthopedic surgery process, from diagnosis and planning to recovery and follow-up care, AI is redefining the patient experience and setting a new standard for outcomes in orthopedic medicine. This powerful partnership between technology and healthcare brings hope for even more groundbreaking advancements in orthopedic surgery, creating a future where every patient receives the highest standard of care.
Top 10 Real-Life Use Cases of AI and Predictive Analytics in Orthopedic Surgery
AI and predictive analytics are transforming orthopedic surgery, providing insights that improve patient care, optimize surgical procedures, and enhance recovery outcomes. Here, we explore ten real-life use cases where AI and predictive analytics are changing orthopedic practices and delivering significant benefits to both patients and healthcare providers.
1. Enhancing Preoperative Planning with Predictive Analytics
How AI Improves Surgical Preparation
In orthopedic surgery, preoperative planning is crucial to ensure successful outcomes. AI and predictive analytics help surgeons analyze patient data, including medical history, imaging, and even genetic information, to anticipate potential challenges and customize surgical approaches. With AI models predicting complications, surgeons can plan around high-risk areas, resulting in a safer, more precise procedure.
Benefits for Patients
- Increased Surgical Success: Tailored approaches reduce complications during surgery.
- Better Preparation: Patients gain insights into their unique risks, which helps set realistic expectations for recovery.
- Reduced Operating Time: More accurate planning streamlines the surgery, reducing time under anesthesia.
2. Early Detection of Osteoarthritis Through AI Diagnostics
Detecting Degenerative Changes Early
Osteoarthritis can lead to severe joint damage if not detected early. AI-enhanced imaging tools analyze X-rays, MRIs, or CT scans to identify subtle, early signs of osteoarthritis, often years before symptoms appear. These AI systems provide insights that help doctors recommend lifestyle changes, medications, or physical therapy before the condition worsens.
Benefits for Patients
- Timely Intervention: Early detection allows patients to manage osteoarthritis with non-surgical treatments.
- Prolonged Joint Health: By slowing progression, patients can delay or even avoid joint replacement surgery.
- Reduced Pain and Improved Mobility: Early treatments help manage symptoms and maintain movement quality.
3. Optimizing Total Joint Replacement with AI-Driven Implant Selection
Personalizing Implants for Better Outcomes
AI tools analyze patient-specific factors, such as body type, activity level, and bone structure, to help select the ideal implant for joint replacement surgeries. For example, in hip or knee replacements, AI-driven implant selection can lead to better fit and longevity, reducing the need for future revision surgeries.
Benefits for Patients
- Improved Implant Fit and Function: Personalization reduces discomfort and enhances mobility.
- Extended Implant Lifespan: Optimized implants last longer, especially for active patients.
- Lowered Risk of Revision Surgery: Fewer adjustments or replacements mean less disruption for the patient.
4. Predicting Spinal Fusion Surgery Outcomes
Enhancing Decision-Making in Complex Spine Surgeries
Spinal fusion surgery is complex, with a high risk of complications. Predictive analytics models help surgeons evaluate patient-specific risk factors—like bone density, smoking history, or previous surgeries—to predict outcomes for fusion success. This insight guides decisions on alternative or supplemental treatments, optimizing results for each patient.
Benefits for Patients
- Higher Fusion Success Rates: Customized approaches improve bone healing and fusion success.
- Reduced Recovery Time: Better predictions allow surgeons to use techniques that minimize recovery duration.
- Lower Risk of Chronic Pain: Accurate planning and execution reduce the likelihood of postoperative pain.
5. Postoperative Pain Management Using AI Algorithms
Tailoring Pain Relief Plans for Faster Recovery
AI systems use data from past patients to predict pain levels and recovery timelines, helping doctors create customized pain management plans. For instance, AI can indicate when a patient may require additional medication or alternative pain relief, such as nerve blocks, reducing dependency on opioids and supporting faster recovery.
Benefits for Patients
- Optimized Pain Relief: Personalized plans help manage pain without excessive medication.
- Reduced Risk of Opioid Dependency: AI supports non-opioid alternatives, minimizing dependency risks.
- Improved Recovery Experiences: Lower pain levels enable patients to participate more actively in rehabilitation.
6. AI-Powered Robotics for Precision in Knee Replacement
Assisting Surgeons with Robotic Accuracy
In knee replacement surgeries, AI-driven robotic systems assist surgeons by providing real-time guidance on incision angles, ligament balance, and bone alignment. These robotic systems use patient data to refine the surgeon’s precision, making minimally invasive techniques more accurate and reducing recovery times.
Benefits for Patients
- Less Invasive Procedures: Smaller incisions result in reduced tissue damage and faster healing.
- Enhanced Accuracy: Robotic assistance leads to better alignment and implant positioning.
- Shorter Recovery Time: Precise surgeries cause less trauma, promoting a quicker return to daily activities.
7. Real-Time Monitoring of Recovery Progress
Tracking Recovery Using Predictive Analytics
AI and predictive analytics track patient recovery progress through digital health records, wearable devices, and patient-reported outcomes. By assessing factors like pain levels, mobility, and physical activity, AI models detect signs of delayed recovery, allowing healthcare providers to intervene early.
Benefits for Patients
- Proactive Adjustments to Care: Early detection of recovery issues means faster solutions.
- Improved Motivation: Patients see their progress, which encourages adherence to recovery routines.
- Personalized Rehabilitation Plans: Custom plans ensure the recovery process matches each patient’s progress.
8. Reducing Complications in Hip Fracture Surgery
Using AI to Identify High-Risk Patients
Elderly patients undergoing hip fracture surgery often face a high risk of complications. AI systems evaluate risk factors such as age, bone density, and pre-existing conditions to predict which patients might experience postoperative complications. This allows healthcare providers to monitor vulnerable patients more closely and provide additional support.
Benefits for Patients
- Better Preparedness for Surgery: Preoperative interventions reduce risk.
- Improved Postoperative Monitoring: High-risk patients receive extra care, reducing complications.
- Enhanced Recovery Outcomes: Proactive care adjustments ensure a smoother recovery process.
9. Improving Rehabilitation Through Predictive Analytics
Creating Data-Driven Rehab Programs
After orthopedic surgery, rehabilitation is key to regaining full function. Predictive analytics use historical data to create tailored rehabilitation plans based on patient age, physical condition, and type of surgery. These models guide physical therapists in designing exercise routines that maximize recovery and minimize the risk of injury.
Benefits for Patients
- Faster Return to Normal Activity: Rehab plans match each patient’s needs for effective recovery.
- Reduced Risk of Re-Injury: Customized exercises protect healing tissues from strain.
- Better Physical Function: Patients regain strength, balance, and mobility more efficiently.
10. Managing Surgical Workflow and OR Scheduling
Using AI to Optimize Surgical Schedules
AI models streamline operating room (OR) scheduling by predicting surgery durations, staff needs, and equipment requirements. By analyzing these variables, hospitals can optimize OR availability, reducing delays and maximizing patient throughput, especially for high-demand orthopedic surgeries.
Benefits for Patients
- Reduced Waiting Times: Improved scheduling means faster access to surgery.
- Smoother Hospital Experiences: Fewer delays create a better patient journey from admission to recovery.
- Efficient Care: Streamlined OR scheduling supports timely surgery, reducing stress for patients and their families.
FAQ on AI and Predictive Analytics in Orthopedic Surgery
How is AI used in orthopedic surgery?
AI in orthopedic surgery assists in preoperative planning, imaging, and even surgical procedures. It analyzes large amounts of data to help surgeons make better decisions, predict possible complications, and improve precision in areas like joint replacement and spinal surgeries.
Can AI help reduce complications in surgery?
Yes, AI can identify patient-specific risk factors, helping surgeons adjust their approach to minimize complications. By analyzing data from past cases, AI predicts potential risks and helps healthcare teams take preventive measures before, during, and after surgery.
How does predictive analytics improve patient outcomes?
Predictive analytics assesses patient data to forecast outcomes based on personal health information, lifestyle, and genetics. This enables more personalized care plans, allowing surgeons to address individual needs and anticipate recovery patterns for better outcomes.
Is AI used for diagnosing orthopedic conditions?
Absolutely. AI-powered tools are widely used to interpret imaging like X-rays and MRIs, identifying issues such as fractures, tears, and signs of arthritis. AI can spot early signs of conditions that are sometimes missed by the human eye, allowing for timely intervention.
How does AI improve joint replacement surgeries?
In joint replacements, AI helps select the most suitable implant and determines precise positioning and alignment. This level of customization improves the function and durability of implants, leading to better mobility and a more comfortable fit for the patient.
Can AI and predictive analytics shorten recovery times?
By predicting individual recovery paths, AI allows healthcare providers to develop targeted rehabilitation plans. Patients receive personalized recommendations that match their unique pace of healing, often leading to quicker and more effective recovery.
Are robotic systems used with AI in orthopedic procedures?
Yes, robotic systems often work alongside AI to support precision in surgery. In procedures like knee replacements, AI-guided robots help surgeons make accurate cuts and alignments, which improves outcomes and reduces trauma to surrounding tissue.
How does AI support pain management after surgery?
AI-driven models help predict pain levels, allowing doctors to create customized pain management plans. This approach helps manage discomfort without excessive reliance on opioids, reducing potential dependency and improving patient comfort during recovery.
What is the role of predictive analytics in spinal surgeries?
In spinal fusion and other complex spinal procedures, predictive analytics helps assess risk factors like bone density and previous injuries. This information allows surgeons to tailor their approach and take preventive steps to improve the chances of successful fusion and recovery.
Is AI technology helpful for elderly patients undergoing orthopedic surgery?
AI technology is particularly valuable for elderly patients, who may face higher surgical risks. By identifying potential complications early and adjusting care accordingly, AI supports safer procedures and helps reduce post-surgical risks like infection or delayed healing.
Can predictive analytics assist with operating room scheduling?
Yes, predictive analytics helps hospitals optimize OR schedules by estimating the length of surgeries and resource needs. This makes it easier to manage high-demand surgeries and reduces patient waiting times, improving overall patient flow.
How are AI tools used in preoperative assessments?
AI tools analyze a patient’s medical history, current health, and lifestyle factors to assess their surgical readiness. This supports better planning and helps ensure that patients are fully prepared, minimizing risks associated with the procedure.
Are AI and predictive analytics used in rehabilitation?
AI and predictive analytics provide valuable insights for rehabilitation planning, helping physical therapists create individualized programs based on the patient’s specific condition and progress. This customization improves the effectiveness of post-surgery rehabilitation.
How do AI-powered imaging tools detect orthopedic issues?
AI-powered imaging tools use algorithms to analyze scans and detect abnormalities that may not be obvious to the naked eye. This technology is especially helpful in identifying subtle fractures or early-stage joint degeneration, allowing for earlier treatment.
What is the future of AI and predictive analytics in orthopedic surgery?
The future includes advancements in robotic precision, sensory feedback in prosthetics, and even brain-computer interfaces for better movement control. AI will continue to offer new levels of customization and prediction, making orthopedic surgery safer and more effective.