Deep Brain Stimulation Surgery Enhanced by AI Technology
- Enhanced precision: AI aids in accurately placing electrodes.
- Personalized treatment: Tailors stimulation based on patient data.
- Real-time monitoring: AI adjusts settings dynamically during surgery.
- Machine learning: Analyzes brain signals to optimize treatment.
- Robotic assistance: AI-driven robots assist in electrode placement.
- Predictive analytics: AI forecasts patient outcomes, reducing risks.
Deep Brain Stimulation (DBS) is a revolutionary neurosurgical procedure. It involves implanting electrodes in specific areas of the brain to treat neurological conditions such as Parkinson’s disease, essential tremor, and dystonia. In recent years, artificial intelligence (AI) has significantly enhanced DBS techniques, making the procedure more precise and adaptable. In this article, we explore the intricate role AI plays in improving DBS outcomes and discuss its potential to revolutionize neurological treatments.
The Role of AI in DBS Surgery
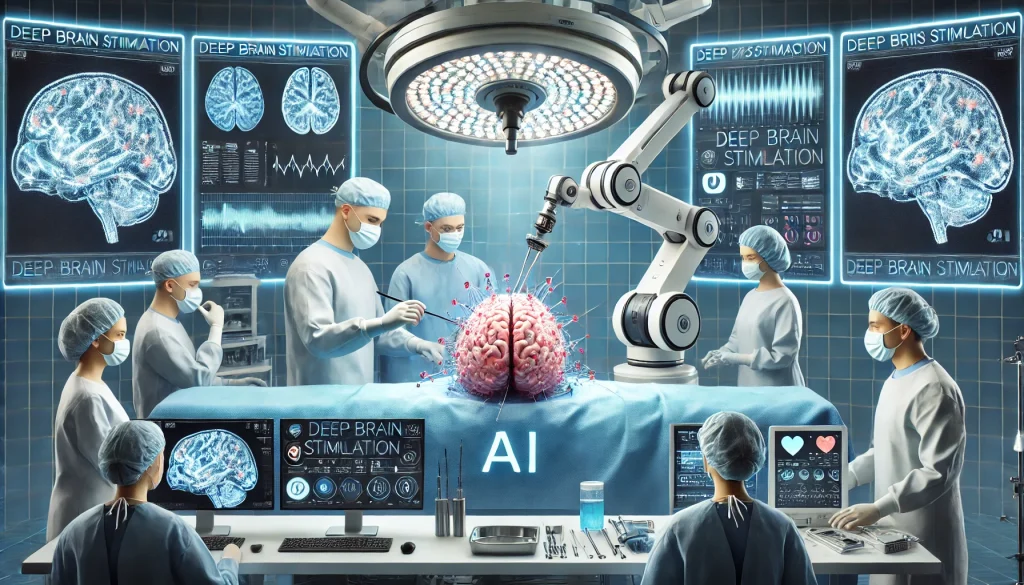
AI’s integration into DBS has reshaped how surgeons approach this complex procedure. The use of machine learning algorithms, neural networks, and data-driven models has improved surgical precision, patient outcomes, and overall procedural safety.
AI and Pre-Surgical Planning
AI aids in preoperative planning by:
- Analyzing medical history and brain imaging: Machine learning models analyze patient-specific brain scans, pinpointing the most effective regions for electrode placement.
- Predictive modeling: AI creates predictive models that forecast patient responses to DBS, helping doctors tailor treatment plans.
Intraoperative Use of AI
AI also plays a crucial role during the actual DBS surgery. These advancements provide real-time data and improve accuracy:
- Robot-assisted surgery: AI-driven robotic systems ensure precise placement of electrodes, minimizing human error.
- Real-time monitoring: AI algorithms track brain activity, allowing surgeons to adjust electrode placement dynamically.
Post-Surgical Optimization Using AI
AI continues to be valuable after the surgery is completed. Its applications include:
- Adaptive programming of stimulators: AI helps personalize the electrical stimulation delivered by the DBS device based on patient feedback and neural signals.
- Monitoring and adjusting stimulation settings: AI-powered platforms monitor the patient’s symptoms and adjust the DBS settings to optimize therapeutic outcomes over time.
Benefits of AI in Deep Brain Stimulation
Improved Precision
AI allows for a more precise targeting of brain regions, minimizing side effects and enhancing treatment efficacy. This precision reduces the chances of complications, offering patients better outcomes.
Customization of Treatment
Each patient’s brain is unique. AI tailors DBS settings to individual neural patterns, offering a personalized approach that manual methods cannot match. Customization ensures that the stimulation is both effective and comfortable.
Real-Time Feedback and Adjustments
With the help of AI, DBS can now respond to real-time changes in brain activity. This dynamic adjustment capability leads to more efficient symptom control, especially in conditions like Parkinson’s where symptoms fluctuate throughout the day.
AI Technologies Used in DBS
The technologies fueling AI’s contributions to DBS are varied, each bringing distinct advantages to different stages of the procedure.
Machine Learning and Data Analytics
Machine learning algorithms play a crucial role in analyzing patient data, predicting outcomes, and optimizing electrode placement. These algorithms are trained on massive datasets, making them more accurate over time.
Robotic-Assisted Systems
Robotic systems equipped with AI ensure that the surgery is as minimally invasive and accurate as possible. These systems can map the brain in real-time and guide surgeons in placing electrodes with sub-millimeter precision.
Neural Networks and Brain Mapping
Neural networks assist in mapping the brain, identifying areas that will most benefit from stimulation. These networks use data from prior DBS surgeries to predict the best areas for intervention in new patients.
AI-Driven Advancements in DBS Research
AI is not just improving current DBS procedures but is also pushing the boundaries of what’s possible. Ongoing research and development are opening new avenues for DBS.
Closed-Loop Systems
Unlike traditional open-loop systems where stimulation is constant, AI-powered closed-loop systems adjust the stimulation based on real-time brain signals. This leads to more efficient treatment, reducing side effects and prolonging battery life.
Integration with Neuroprosthetics
AI’s ability to decode brain signals is paving the way for advanced neuroprosthetics. By interpreting neural activity, AI can help develop prosthetics that respond more naturally to the patient’s brain signals.
Predictive Outcomes with AI Models
AI is helping surgeons predict patient outcomes more accurately. By analyzing data from thousands of previous DBS surgeries, AI can forecast the likelihood of success and potential risks, aiding in the decision-making process.
Challenges and Limitations of AI in DBS
While AI has introduced remarkable advancements in DBS, several challenges remain.
Data Quality and Quantity
AI models require vast amounts of high-quality data to function effectively. In DBS, collecting standardized data across different patients and conditions is a challenge, which may limit the accuracy of AI predictions.
Ethical Concerns
The use of AI in neurosurgery raises ethical concerns, particularly around the autonomy of decision-making. Ensuring that AI tools enhance rather than replace human judgment is crucial to maintaining trust in the technology.
Cost and Accessibility
AI-powered DBS systems are expensive, potentially limiting access to this advanced treatment for many patients. Developing cost-effective solutions and improving accessibility should be a focus for future research.
Advancements in AI for Deep Brain Stimulation Surgery
Expanded Applications
AI’s role in DBS is expected to expand beyond traditional neurological disorders. Research is exploring AI-enhanced DBS for treating psychiatric conditions such as depression and obsessive-compulsive disorder.
Improved Closed-Loop Systems
Future AI-driven closed-loop systems may be fully autonomous, adjusting stimulation settings continuously without human intervention. This would allow for seamless, real-time management of symptoms.
AI-Driven Brain-Computer Interfaces (BCI)

The integration of AI with BCIs holds immense potential. AI could enable DBS devices to communicate with external systems, allowing for more interactive treatments that adapt to a broader range of neurological signals.
The integration of AI into Deep Brain Stimulation Surgery is transforming how we approach neurological treatments. By improving precision, customization, and real-time responsiveness, AI has brought DBS into a new era of innovation. As research progresses, we can expect even greater advancements in patient outcomes, making AI an indispensable tool in modern neurosurgery.
Top 10 Real-Life Use Cases of AI in Deep Brain Stimulation Surgery
Artificial intelligence has brought transformative changes to Deep Brain Stimulation (DBS) surgery, enhancing precision, treatment customization, and overall outcomes. Below, we explore ten real-life use cases where AI is being used in DBS surgery, along with the detailed benefits of each.
1. AI-Assisted Pre-Surgical Planning
AI Algorithms in Imaging Analysis
AI algorithms analyze brain scans (such as MRI and CT) to map out the specific regions of the brain that require stimulation. This detailed analysis helps in identifying the precise location for electrode placement.
Benefits
- Enhanced accuracy: AI reduces the margin of error in targeting the correct area.
- Time efficiency: Automated imaging analysis speeds up the pre-surgical planning process.
2. Real-Time Electrode Placement with AI
Robotic Assistance
AI-driven robotic systems are now assisting surgeons in placing electrodes during DBS procedures. These systems use real-time feedback and guidance from AI to ensure that electrodes are inserted with sub-millimeter precision.
Benefits
- Minimized human error: Robotic systems make electrode placement more precise than manual methods.
- Improved safety: Precision placement reduces the likelihood of damaging surrounding brain tissue.
3. AI-Driven Closed-Loop Stimulation Systems
Responsive Stimulation
Closed-loop systems powered by AI continuously monitor brain activity and adjust the stimulation accordingly. These systems can react in real-time to changes in the patient’s symptoms or neural signals.
Benefits
- Dynamic adjustments: Real-time changes in stimulation lead to more effective symptom management.
- Reduced side effects: Tailoring the stimulation reduces overstimulation or unnecessary electrical impulses.
4. Personalized DBS Treatment Plans with AI
Data-Driven Customization
Machine learning models analyze each patient’s brain signals, symptoms, and previous treatments to create personalized DBS programs. AI can adjust the intensity and location of stimulation based on patient-specific data.
Benefits
- Tailored treatment: AI ensures each patient receives a unique and optimized treatment.
- Increased efficacy: Personalized settings lead to better therapeutic outcomes.
5. AI-Based Outcome Prediction
Predictive Analytics
AI models can predict how effective DBS will be for a particular patient by analyzing data from past surgeries and patient outcomes. This allows for better decision-making before the surgery even begins.
Benefits
- Improved success rates: AI predictions allow surgeons to select the most promising candidates for DBS.
- Informed decision-making: Surgeons can anticipate potential complications and adjust plans accordingly.
6. Post-Surgical AI Monitoring Systems
Ongoing Symptom Tracking
AI-driven platforms monitor patients post-surgery, tracking their neurological responses and symptoms. These systems help in adjusting stimulation settings remotely and automatically.
Benefits
- Continuous care: AI monitors patient progress without the need for frequent hospital visits.
- Optimal stimulation settings: Real-time tracking ensures that the stimulation is always in the best range for symptom control.
7. AI-Assisted Brain Mapping
Neural Networks for Brain Mapping
AI systems use neural networks to map the brain’s electrical activity, identifying the areas most responsive to stimulation. This technology helps refine the placement of DBS electrodes for each individual patient.
Benefits
- Greater precision: Accurate brain mapping leads to improved electrode placement.
- Minimization of side effects: Correct targeting ensures only the affected areas are stimulated.
8. Adaptive AI for Symptom Fluctuations
Real-Time Adjustments
AI can dynamically adjust stimulation based on daily or even hourly fluctuations in a patient’s symptoms. This is particularly useful for conditions like Parkinson’s disease, where symptoms can vary greatly throughout the day.
Benefits
- Continuous symptom control: AI maintains consistent symptom relief despite fluctuations.
- Reduction of unnecessary stimulations: AI avoids overstimulating the brain during low-symptom periods.
9. AI and Neuroprosthetics in DBS
Integration with Neuroprosthetics
AI helps integrate DBS with neuroprosthetics to assist patients with motor control issues. AI-powered neuroprosthetics interpret brain signals and work in tandem with DBS to improve motor functions.
Benefits
- Enhanced motor control: Patients experience better coordination and mobility.
- Increased independence: Neuroprosthetics, controlled by AI, improve the quality of life for patients with motor impairments.
10. AI-Enhanced Electrode Design
Smart Electrode Development
AI is being used to design smarter, more efficient DBS electrodes. These electrodes can deliver more precise stimulation and reduce the need for frequent adjustments or replacements.
Benefits
- Longer electrode lifespan: AI-designed electrodes are more durable and effective.
- Reduced surgical interventions: Patients require fewer electrode adjustments, lowering the need for follow-up surgeries.
FAQ: AI in Deep Brain Stimulation Surgery
What role does AI play in DBS surgery?
AI is used throughout the DBS process, from planning to surgery and post-operative care. It helps analyze brain scans, predict outcomes, and adjust stimulation settings during and after surgery.
How does AI help with electrode placement in DBS?
AI assists in placing electrodes with precision by analyzing brain images and guiding robotic systems during surgery. This improves accuracy and minimizes risks associated with human error.
Can AI improve patient outcomes in DBS surgery?
Yes, AI personalizes treatment by analyzing patient data, adjusting stimulation settings in real-time, and monitoring patient responses, leading to better outcomes and symptom management.
How does AI monitor patients after DBS surgery?
AI-powered systems track patient symptoms continuously after the surgery. They adjust the stimulation settings based on real-time feedback from the brain, providing ongoing symptom control.
What is AI-driven closed-loop stimulation in DBS?
Closed-loop systems use AI to monitor brain activity and adjust the electrical stimulation dynamically. This ensures that the treatment responds to changes in the patient’s condition without manual intervention.
Is AI involved in pre-surgical planning for DBS?
Yes, AI helps in pre-surgical planning by analyzing brain scans and mapping the areas that need stimulation. This makes the planning process more accurate and tailored to the patient’s needs.
What kind of data does AI use to customize DBS treatment?
AI uses brain scans, patient history, real-time brain activity, and symptoms to create personalized DBS treatment plans. This data helps in optimizing electrode placement and stimulation settings.
How does AI help in predicting the success of DBS surgery?
AI analyzes large datasets from previous DBS surgeries to predict outcomes. It helps surgeons assess the likelihood of success and potential risks, allowing for informed decision-making before surgery.
Can AI help reduce side effects in DBS?
Yes, AI can reduce side effects by adjusting stimulation settings in real-time based on the patient’s brain signals. This ensures that the stimulation is always within the optimal range for symptom control.
Does AI replace the need for human surgeons in DBS?
AI does not replace human surgeons but acts as a tool to assist them. It enhances precision and provides data-driven insights that help surgeons make more informed decisions.
How does AI contribute to post-surgical care in DBS?
AI-driven platforms monitor patient symptoms after surgery and adjust stimulation settings remotely. This reduces the need for frequent follow-up visits and allows for continuous symptom management.
What are the benefits of using AI in DBS for neurological conditions like Parkinson’s?
AI provides personalized treatment, real-time adjustments, and improved precision in electrode placement, all of which contribute to better symptom control for neurological conditions such as Parkinson’s disease.
Can AI be used for other conditions besides Parkinson’s in DBS?
Yes, AI is also being explored for other conditions such as dystonia, essential tremor, and even psychiatric disorders like depression. It helps customize treatment for these conditions as well.
Are AI systems used only during DBS surgery?
No, AI is involved before, during, and after DBS surgery. It helps in planning, real-time electrode placement, and ongoing monitoring of the patient’s condition post-surgery.
What are the limitations of AI in DBS surgery?
Some limitations include the high cost of AI-powered systems, the need for large amounts of patient data, and ethical concerns around decision-making autonomy during surgery. These challenges are being addressed with ongoing research and development.