Patient Safety Regulations for AI-Driven Surgery
- FDA approval ensures AI systems are tested for safety in the U.S.
- CE marking confirms compliance with European safety standards.
- Risk management protocols like ISO 14971 protect patients from AI-related hazards.
- Informed consent guarantees patient awareness of AI’s role in surgery.
- Post-market surveillance monitors AI performance after regulatory approval.
Introduction
Artificial intelligence (AI) has made groundbreaking advancements in surgical practices, offering new ways to improve precision, reduce errors, and assist with decision-making. However, with these innovations comes the heightened responsibility to ensure patient safety. As AI technologies evolve, patient safety regulations are critical to protecting patients from potential risks posed by AI systems. These regulations govern the development, testing, and deployment of AI in surgery, ensuring that every system is held to the highest safety standards.
Key Patient Safety Regulations Governing AI in Surgery
AI technologies used in surgery must comply with various patient safety regulations set by authorities like the FDA, CE marking in the European Union, and other global regulatory bodies. These regulations focus on ensuring that AI systems are safe, reliable, and transparent.
Key Regulations:
- FDA (Food and Drug Administration): Oversees medical devices in the U.S., ensuring that AI systems used in surgery meet stringent safety and performance standards.
- CE Marking (EU Medical Devices Regulation): Mandates that AI surgical tools meet European safety, health, and environmental protection requirements.
- ISO 14971: An international standard for managing risks associated with medical devices, focusing on patient safety during the entire lifecycle of AI systems.
- Post-market surveillance: Regulatory bodies often require ongoing monitoring of AI systems after approval to ensure long-term patient safety.
FDA Approval Process for AI Surgical Systems
The FDA plays a crucial role in regulating AI-driven surgical systems in the U.S. All AI-based medical devices must go through a rigorous approval process, often following the 510(k) clearance or PMA (Pre-market Approval) pathways. This ensures that the technology is safe and effective for its intended use.
FDA Key Approval Pathways:
- 510(k) clearance: Applied to AI technologies that are substantially equivalent to existing devices.
- Pre-market Approval (PMA): A more stringent process required for high-risk devices, often used for groundbreaking AI systems that don’t have existing counterparts.
- Clinical trials: AI systems must undergo clinical trials to demonstrate that they provide a benefit without introducing unnecessary risks to patient safety.
CE Marking in the European Union
CE Marking is essential for the deployment of AI-driven surgical systems in the European Union. This certification proves that AI systems conform to the Medical Devices Regulation (MDR), ensuring that they meet safety, health, and environmental requirements before being used in healthcare settings.
CE Marking and AI in Surgery:
- Conformity assessment: AI systems must pass thorough testing to ensure they meet safety and performance standards set by the MDR.
- Risk management: Compliance with ISO 14971 ensures that AI surgical tools manage risks appropriately, protecting patient safety at all stages.
- Post-market surveillance: AI systems approved under CE marking are subject to ongoing scrutiny to ensure continued compliance with safety standards.
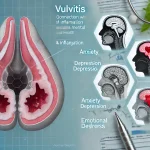
AI in Surgery: Addressing Ethical and Regulatory Challenges
One of the most pressing concerns surrounding AI in surgery is the ethical responsibility of using machine learning algorithms in life-critical procedures. AI must work within ethical boundaries, ensuring patient autonomy, maintaining transparency, and mitigating bias in decision-making processes. Patient safety is intertwined with ethical AI usage, and regulatory frameworks are designed to uphold these principles.
Ethical Considerations:
- Informed consent: Patients must be fully aware of how AI is used during their procedure, and their data rights must be respected.
- Bias in AI: Regulations must ensure that AI algorithms are trained on diverse datasets to prevent biases that could lead to unequal treatment outcomes.
- Accountability: Surgeons remain ultimately responsible for AI-driven decisions, ensuring human oversight during surgery.
Risk Management in AI Surgical Systems
AI surgical systems must comply with comprehensive risk management protocols to safeguard patient safety. This process begins with risk identification, followed by risk assessment and mitigation strategies. Regulatory bodies like the FDA and the EU MDR require developers to follow risk management standards such as ISO 14971 throughout the AI system’s lifecycle.
Risk Management Strategies:
- Risk identification: Assessing potential hazards posed by AI during surgery, including system failures and data inaccuracies.
- Mitigation measures: Implementing fail-safes that allow surgeons to override AI decisions when necessary.
- Continuous monitoring: Ensuring that real-time data is used to track AI system performance during surgery to prevent potential safety issues.
Post-Market Surveillance and AI in Surgery
Even after an AI surgical system is approved, post-market surveillance plays a vital role in ensuring that the system continues to operate safely. Regulatory bodies require AI manufacturers to monitor the system’s performance in real-world settings to detect any unforeseen risks or complications.
Key Elements of Post-Market Surveillance:
- Real-time performance tracking: Monitoring the AI system’s outcomes to ensure consistent patient safety.
- Adverse event reporting: Reporting any complications or malfunctions that arise during surgical use.
- Periodic reviews: Conducting audits to ensure the AI system continues to meet regulatory standards.
Data Integrity and AI in Surgery
Ensuring data integrity is another critical element of patient safety in AI surgery. AI systems rely on vast amounts of patient data to make informed decisions, and any breach or corruption of this data could have catastrophic consequences during surgery. Regulatory bodies enforce stringent guidelines to protect the integrity and security of patient data used by AI systems.
Data Integrity Measures:
- Encryption: All data used by AI systems should be encrypted to protect it from unauthorized access.
- Anonymization: Ensuring that patient data used in AI systems is anonymized to comply with data privacy regulations such as GDPR and HIPAA.
- Audit trails: Maintaining clear records of how AI systems use and process data to ensure transparency and traceability.
Informed Consent and Patient Safety in AI Surgery
Obtaining informed consent is essential when using AI in surgery. Patients need to understand the role of AI in their treatment, the potential benefits, and any risks involved. Ensuring that patients are fully aware of how their data will be used and protected is a crucial aspect of maintaining trust in AI surgical systems.
Informed Consent Elements:
- Transparency: Patients must be informed about how AI systems will assist in their surgery and what role the surgeon plays in overseeing the technology.
- Data usage: Clear explanations about how patient data is collected, stored, and used by the AI system.
- Risk disclosure: Providing patients with information about any potential risks associated with the use of AI in their procedure.
The Role of AI in Reducing Surgical Errors
AI systems are instrumental in reducing surgical errors by analyzing real-time data, providing decision support, and offering precision tools. However, to ensure these systems perform as expected, they must comply with patient safety regulations that govern their design, testing, and clinical use.
Benefits of AI in Reducing Errors:
- Real-time data analysis: AI systems can process vast amounts of data quickly, providing surgeons with crucial insights during complex procedures.
- Precision: AI-powered tools allow for more accurate surgical techniques, minimizing the risk of human error.
- Predictive analytics: AI can predict potential complications based on patient data, helping surgeons avoid mistakes before they happen.
Global Regulations and Harmonization
One of the challenges facing AI in surgery is the lack of global harmonization in patient safety regulations. While the FDA and CE marking provide clear guidelines in the U.S. and Europe, other regions have different standards. Moving toward global regulatory alignment would help streamline the approval process and ensure that AI systems meet universal safety standards.
Benefits of Global Harmonization:
- Faster approvals: Global alignment would reduce the time needed for AI systems to be approved in multiple regions.
- Standardized safety: Ensuring that all AI surgical systems adhere to the same patient safety requirements across borders.
- Enhanced collaboration: Facilitating better cooperation between regulatory bodies, manufacturers, and healthcare providers.
Future Trends in AI Surgery and Patient Safety
The future of AI in surgery will continue to be shaped by evolving patient safety regulations. As AI becomes more sophisticated, regulatory bodies will need to adapt to new challenges, including adaptive AI systems, real-time data compliance, and autonomous surgical tools. Future regulations will likely focus on continuous monitoring, greater transparency, and real-time validation of AI systems to ensure ongoing patient safety.
Key Trends:
- Adaptive AI: Systems that learn and evolve will require ongoing validation to ensure they continue to meet safety standards.
- Real-time compliance: Future regulations may include real-time monitoring systems that ensure AI remains compliant during surgeries.
- Ethical AI development: Ensuring that AI systems are designed and tested in ways that uphold patient safety and ethical medical practices.
Conclusion
As AI continues to transform surgical practices, patient safety regulations must evolve to ensure that these innovations do not compromise patient well-being. From FDA approval to CE marking, regulatory bodies around the world are working to ensure that AI systems are safe, effective, and ethical. By adhering to these standards, AI can fulfill its potential to improve patient outcomes and revolutionize surgical care while maintaining the highest safety standards.
Top 10 Real-Life Use Cases: AI in Surgery and Patient Safety Regulations
1. da Vinci Surgical System: Regulatory Framework and Safety Standards
The da Vinci Surgical System is a widely recognized robotic platform that uses AI to assist surgeons in performing minimally invasive surgeries. This system underwent rigorous FDA 510(k) clearance and CE marking to ensure it met the highest patient safety standards.
Benefits:
- FDA-approved precision tools that reduce surgical error.
- Minimally invasive techniques improve patient recovery times.
- Ongoing post-market surveillance ensures continuous compliance with safety standards.
2. ZAP-X Radiosurgery Platform: Non-Invasive Tumor Treatment
The ZAP-X Radiosurgery Platform uses AI to deliver non-invasive brain tumor treatments. It adheres to stringent FDA and CE safety regulations that ensure it targets tumors with high precision while minimizing risks to surrounding tissues.
Benefits:
- Non-invasive surgery reduces recovery time and surgical risks.
- Real-time AI guidance improves treatment accuracy.
- Data protection standards ensure patient safety and privacy during treatments.
3. CyberKnife: AI-Guided Radiosurgery
The CyberKnife system provides robotic-assisted, AI-driven radiosurgery for treating tumors. It complies with FDA’s pre-market approval (PMA) process, ensuring that the technology delivers precise, targeted radiation while maintaining strict safety guidelines.
Benefits:
- FDA-approved AI technology ensures precise targeting of tumors.
- Reduced collateral damage to healthy tissue, improving patient outcomes.
- Safety protocols verified through extensive clinical trials.
4. HeartFlow FFRct: AI-Driven Cardiovascular Diagnosis
The HeartFlow FFRct uses AI to analyze coronary CT scans, providing a non-invasive diagnosis of coronary artery disease. It has passed FDA 510(k) clearance and CE marking to meet safety regulations for cardiovascular diagnostics.
Benefits:
- Non-invasive diagnosis reduces the need for risky catheter-based procedures.
- Data compliance ensures patient information is handled securely.
- Proven clinical accuracy through rigorous trials and regulatory approval.
5. Monarch Platform: AI-Assisted Bronchoscopy
The Monarch Platform uses AI for minimally invasive bronchoscopic procedures. To maintain patient safety, the system complies with both FDA approval and ISO 14971 risk management standards to ensure it safely navigates lung pathways and reduces surgical risks.
Benefits:
- Enhanced precision in diagnosing and treating lung diseases.
- Minimally invasive methods reduce recovery times.
- Real-time AI assistance enhances patient safety during complex procedures.
6. GI Genius: AI for Colonoscopy and Early Cancer Detection
GI Genius is an AI-driven tool that assists doctors during colonoscopies by detecting polyps and early signs of colorectal cancer. The device underwent FDA 510(k) clearance to ensure it complies with strict patient safety guidelines.
Benefits:
- AI-assisted detection of polyps leads to early cancer intervention.
- FDA-approved technology ensures reliability and accuracy.
- Improved patient outcomes due to early diagnosis and treatment.
7. IDx-DR: Autonomous AI for Diabetic Retinopathy
The IDx-DR system is an autonomous AI diagnostic tool for detecting diabetic retinopathy. It became the first autonomous AI system to receive FDA clearance after proving that it could safely and accurately diagnose eye conditions without clinician involvement.
Benefits:
- Autonomous diagnostics improve access to care in remote areas.
- Stringent FDA safety protocols ensure patient trust in AI results.
- Informed consent and data compliance are integral to the system’s use.
8. Medtronic Hugo: AI-Assisted Robotic Surgery
The Medtronic Hugo robotic system combines AI and robotics to assist surgeons during minimally invasive procedures. It complies with CE marking in Europe, and the system follows ISO 14971 risk management protocols to maintain patient safety during operations.
Benefits:
- Real-time AI assistance improves the accuracy of surgical procedures.
- Regulatory approval ensures the system meets safety standards.
- Continuous post-market monitoring ensures safe long-term use.
9. SurgiBot: Portable Robotic Surgery and Data Compliance
The SurgiBot system provides portable robotic surgery solutions powered by AI. To comply with FDA and HIPAA regulations, SurgiBot incorporates data encryption and privacy protocols to ensure patient data security during surgical procedures.
Benefits:
- Portable AI-assisted surgery broadens access to advanced care.
- Strict adherence to data privacy regulations ensures patient safety.
- Ongoing monitoring ensures compliance with global safety standards.
10. ProFound AI: Breast Cancer Detection through AI
ProFound AI aids radiologists by analyzing mammography images for early signs of breast cancer. This system passed FDA 510(k) clearance and CE marking in the European Union, meeting the required safety and performance standards.
Benefits:
- AI-driven analysis improves early detection rates for breast cancer.
- Regulatory approval ensures that the system adheres to safety protocols.
- Anonymized data processing protects patient privacy during diagnostics.
FAQ on AI in Surgery and Patient Safety Regulations
How does AI improve surgical precision?
AI helps surgeons by analyzing large sets of data in real-time, assisting with decision-making and offering more precise control during complex procedures. It reduces the likelihood of human error and aids in complex surgeries requiring high precision.
What role does the FDA play in AI surgical systems?
The FDA is responsible for evaluating and approving AI-driven surgical systems in the U.S. They ensure that the technology meets safety standards through clinical trials and testing before it can be used in healthcare settings.
Why is CE marking important for AI in surgery?
CE marking certifies that AI-driven medical devices used in the European Union meet the necessary safety, health, and environmental protection requirements. It ensures that AI surgical systems are safe for patient use and comply with EU regulations.
How does AI adhere to patient safety regulations?
AI surgical systems must undergo rigorous testing and approval processes, such as FDA or CE marking, to ensure they meet safety standards. These regulations cover everything from risk management to data protection, ensuring patient safety throughout the process.
What is informed consent in AI surgery?
Informed consent means that patients are fully aware of how AI will be used during their surgery. It involves explaining the role AI will play, the potential risks, and how patient data will be used and protected.
How does AI manage risks during surgery?
AI systems are required to comply with international risk management standards like ISO 14971. These standards help identify potential risks, assess their impact, and implement strategies to mitigate any hazards during surgical procedures.
Why is post-market surveillance necessary for AI surgical systems?
Post-market surveillance ensures that AI systems continue to operate safely after they have been approved and deployed. This ongoing monitoring allows manufacturers and regulators to detect any issues that may arise in real-world clinical use.
How are data privacy regulations like HIPAA and GDPR followed in AI surgery?
AI systems in surgery must comply with data protection laws such as HIPAA in the U.S. and GDPR in the EU. These regulations mandate that patient data is encrypted, anonymized, and securely stored to protect against unauthorized access.
How is patient data anonymized in AI surgical systems?
Data anonymization removes personally identifiable information from patient records, ensuring that data used by AI systems cannot be traced back to an individual. This is a key requirement for complying with GDPR and HIPAA regulations.
What is the role of ISO 14971 in AI surgical systems?
ISO 14971 is an international standard for risk management in medical devices. It ensures that AI surgical systems are designed and developed with patient safety in mind, identifying potential risks and implementing measures to prevent harm.
How do AI systems get approval for use in surgery?
AI systems must pass through regulatory approval processes like the FDA’s 510(k) clearance or Pre-market Approval (PMA) pathways, as well as CE marking in Europe. These processes involve testing, clinical trials, and risk assessments to ensure the systems are safe and effective.
Why is accountability important in AI-assisted surgery?
Although AI assists with decision-making, surgeons remain responsible for patient outcomes. AI systems are tools to help surgeons, but human oversight is critical to ensure that decisions align with the best interests of the patient.
What is the impact of AI on reducing surgical errors?
AI systems reduce surgical errors by providing real-time data analysis, precision tools, and predictive capabilities. This can help surgeons avoid complications, minimize mistakes, and make more informed decisions during surgery.
How are AI surgical systems monitored for long-term safety?
Once approved, AI surgical systems undergo regular audits and post-market surveillance to ensure they continue to operate safely. Any issues that arise are reported to regulatory bodies like the FDA or European health authorities for further investigation.
How does AI ensure fairness and avoid bias in surgical decisions?
AI algorithms are trained on diverse datasets to avoid biased decision-making. Regulatory bodies ensure that AI systems undergo bias testing during the approval process, ensuring that all patients receive equitable care regardless of demographic differences.