Key Ethical Case Studies in AI Surgery Practices
- Accountability: Who is responsible when AI systems fail during surgery?
- Bias: How do biased AI algorithms impact patient outcomes?
- Transparency: Are patients fully informed about AI’s role in their procedures?
- Informed Consent: Do patients understand the risks associated with AI-assisted surgery?
- Patient Safety: How are AI errors managed during critical surgeries?
Introduction
Artificial intelligence (AI) in surgery offers remarkable potential, providing tools that assist with everything from preoperative planning to real-time guidance during procedures. However, the ethical implications of integrating AI in healthcare cannot be ignored. Ethical challenges arise concerning patient safety, accountability, transparency, and biases in decision-making. By examining real-world ethical case studies, we can gain insight into how these dilemmas manifest in practice and how they are addressed. This article explores some of the most critical ethical case studies involving AI in surgery, providing a comprehensive view of the issues at hand.
The Role of AI in Surgery and the Ethical Landscape
AI technologies have transformed the surgical environment, offering precision, data analytics, and improved decision-making. But these advancements also raise concerns about accountability, data privacy, and how AI affects surgeon-patient relationships. Ethical considerations must be at the forefront when implementing AI systems, ensuring that patient welfare is always prioritized.
Case Study 1: Robotic Surgery Malfunction and Patient Safety
AI-powered robotic surgery systems provide high precision in complex procedures, but technical failures can lead to disastrous outcomes. In a case where a robotic surgery system malfunctioned mid-procedure, questions arose about who was responsible for the resulting complications: the surgeon, the software developers, or the hospital?
Key Ethical Issues:
- Accountability: Who is held accountable when AI malfunctions?
- Transparency: Did the patient fully understand the role of AI in the surgery and the risks involved?
- Patient Safety: What safeguards should be in place to protect patients when AI systems fail?
Conclusion:
Hospitals need clear protocols for managing AI malfunctions. Surgeons must remain fully informed of the system’s limitations, and patients must be made aware of potential risks.
Case Study 2: AI Bias in Predictive Surgical Outcomes
AI systems trained on non-diverse datasets can display bias, affecting patient outcomes. A hospital using an AI system to predict surgical success rates found that the system consistently predicted worse outcomes for minority patients, despite their having similar health profiles as non-minority patients. This case sparked a conversation about data representation and fairness in AI development.
Key Ethical Issues:
- Bias: How do biased datasets impact surgical decision-making for minority patients?
- Fairness: Is AI providing equal care for all patient demographics?
- Informed Consent: Were patients made aware of potential biases in the system?
Conclusion:
AI developers must ensure that their systems are trained on diverse datasets. Regular audits are needed to detect and eliminate bias, ensuring fairness in healthcare delivery.
Case Study 3: AI in Preoperative Planning and Patient Autonomy
An AI system was used to recommend surgical approaches based on patient data. However, the surgeon disagreed with the AI’s recommendation and followed their own judgment. The patient later experienced complications, and the family sued, questioning whether the surgeon or the AI was at fault. This case highlights the tension between human expertise and AI recommendations.
Key Ethical Issues:
- Autonomy: Should surgeons always follow AI recommendations, or should human judgment prevail?
- Liability: Who is responsible when AI’s advice is disregarded, and the outcome is poor?
- Trust: How can trust between AI systems and surgeons be fostered?
Conclusion:
Surgeons must balance AI recommendations with their own expertise, but they also need to document their decision-making process thoroughly to protect themselves legally.
Case Study 4: Data Privacy in AI-Assisted Surgery
AI systems often rely on vast amounts of patient data to function, raising concerns about data privacy and security. In a case where an AI system used by a hospital was hacked, patient data was exposed. This breach led to a serious debate about the security measures in place for protecting sensitive health information.
Key Ethical Issues:
- Data Security: How can hospitals ensure the AI systems they use are secure against breaches?
- Patient Consent: Did patients give informed consent for their data to be used by AI systems?
- Transparency: Are patients informed about how their data is stored and used in AI-driven surgical systems?
Conclusion:
Strong encryption and security protocols are essential for safeguarding patient data in AI systems. Patients must also be fully informed about how their data is handled and protected.
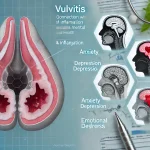
Case Study 5: AI Decision-Making in Life-and-Death Situations
In an emergency surgery scenario, AI systems are sometimes used to make real-time decisions that can affect patient outcomes. In one case, an AI-driven system recommended a high-risk surgery for a critically ill patient. The surgeon followed the AI’s recommendation, but the patient did not survive. This raised questions about the role of AI in critical decision-making and whether the risks were adequately communicated.
Key Ethical Issues:
- Informed Consent: Did the patient and family fully understand the role of AI in the decision?
- Accountability: Should AI take responsibility for decisions, or does it rest solely with the surgeon?
- Risk Management: How can AI systems better communicate the risks associated with their recommendations?
Conclusion:
AI should never replace human judgment in life-and-death situations. Surgeons must retain decision-making authority while using AI as a support tool.
Case Study 6: AI and Resource Allocation in Surgery
An AI system was used to allocate surgical resources such as operating room time and staff availability. However, some surgeons argued that the AI system was unfairly prioritizing certain cases over others, creating delays for critical surgeries. This raised ethical concerns about the fairness and transparency of resource allocation in healthcare.
Key Ethical Issues:
- Fairness: Is the AI system prioritizing surgeries based on patient need or other factors?
- Transparency: Are the criteria for AI decision-making in resource allocation clear and equitable?
- Accountability: Who is responsible when AI decisions lead to delays in urgent care?
Conclusion:
Resource allocation must be handled with fairness, ensuring that AI systems prioritize based on medical need and not arbitrary factors. Regular audits of AI decision-making processes are critical.
Case Study 7: AI in Post-Surgical Recovery Predictions
AI was employed to predict post-surgical recovery times, helping hospitals manage bed availability and patient turnover. However, the system consistently overestimated recovery times for elderly patients, leading to unnecessary extended hospital stays. This case demonstrated the need for more accurate and adaptive AI systems in post-surgical care.
Key Ethical Issues:
- Accuracy: How accurate are AI predictions for different patient demographics?
- Bias: Does the system disproportionately affect elderly or vulnerable patients?
- Patient Welfare: How do inaccurate AI predictions impact patient care and recovery?
Conclusion:
AI systems must be regularly updated and refined to ensure they account for all patient demographics and do not cause unnecessary delays in patient discharge.
Case Study 8: AI-Assisted Robotic Surgery in Pediatric Patients
In pediatric surgery, an AI-driven robotic system was used for a complex operation. The family of the child questioned whether AI-assisted surgery was appropriate for such a young patient, as there were concerns about the system’s ability to handle pediatric anatomy. The ethical debate centered on whether the AI system was designed with children in mind.
Key Ethical Issues:
- Suitability: Is the AI system trained and tested for use on pediatric patients?
- Informed Consent: Did the parents fully understand the role of AI in their child’s surgery?
- Bias: Is the AI system biased against certain age groups, and does it function equally well for pediatric cases?
Conclusion:
AI systems must be rigorously tested for specific patient populations, including pediatric cases, to ensure they are suitable for all age groups.
Case Study 9: AI-Driven Surgical Training and Ethical Concerns
AI was used to train new surgeons in complex procedures, simulating real-life surgeries. While the AI training system was praised for its accuracy, some experienced surgeons raised concerns about over-reliance on AI during training, fearing that new surgeons might not develop essential decision-making skills.
Key Ethical Issues:
- Over-Reliance on AI: Are surgeons becoming too dependent on AI systems during training?
- Skill Development: Does AI training limit the development of critical thinking and problem-solving skills?
- Safety: Are patients at risk if surgeons rely too heavily on AI during live surgeries?
Conclusion:
AI training tools should complement, not replace, traditional hands-on surgical training. Surgeons must develop independent decision-making skills to ensure patient safety.
Case Study 10: AI and Informed Consent in Complex Surgeries
An AI system was used to assist in a complex spinal surgery, but the patient later expressed concern that they had not been properly informed about AI’s role in the procedure. This case highlighted the importance of fully transparent informed consent when AI is used in surgeries, particularly when the system plays a significant role in decision-making.
Key Ethical Issues:
- Transparency: Did the patient fully understand AI’s involvement in the surgery?
- Informed Consent: Was the patient given enough information to make an informed decision?
- Trust: How can trust between surgeons, patients, and AI systems be fostered through clear communication?
Conclusion:
Informed consent must clearly explain AI’s role in surgeries. Surgeons need to ensure patients understand how AI may influence their procedure and outcomes.
Conclusion
Ethical challenges in AI-assisted surgery are multifaceted, ranging from accountability and transparency to fairness and patient autonomy. Each case study presented here underscores the critical importance of maintaining high ethical standards as AI becomes more integrated into surgical practices. As we continue to adopt AI technologies, addressing these ethical issues head-on will be essential to building trust, ensuring patient safety, and promoting equitable healthcare outcomes.
Top 10 Real-Life Use Cases of Ethical Case Studies in AI Surgery
1. AI-Assisted Robotic Surgery Malfunction
A robotic surgical system failed during a delicate procedure, leading to significant complications for the patient. The ethical question revolved around accountability: whether the surgeon, hospital, or the AI manufacturer was responsible for the failure and its consequences.
Key Ethical Concerns:
- Accountability: Determining who is responsible when AI systems fail.
- Patient Safety: How to manage risks in surgeries relying on AI systems.
- Transparency: Did the patient fully understand the risks of AI use?
Benefits:
- Clear protocols for managing AI malfunctions.
- Increased focus on transparency with patients.
- Enhanced safety measures and checks for AI-driven surgeries.
2. Bias in AI Predicting Surgical Outcomes
An AI system used to predict surgical success showed consistent bias against minority groups, resulting in fewer surgical recommendations for these patients. The bias highlighted the lack of diversity in the training data, raising ethical concerns about fairness.
Key Ethical Concerns:
- Bias: Unintended discrimination in healthcare delivery.
- Fairness: Ensuring equal treatment and care for all patient groups.
- Data Representation: The need for diverse datasets in AI training.
Benefits:
- Improved awareness of AI biases.
- Encourages developers to use diverse datasets.
- Increased audits for fairness and equality in AI outcomes.
3. AI in Preoperative Decision-Making
In a complex case, AI recommended a specific surgical approach, but the surgeon chose a different method. After complications arose, questions of liability emerged regarding whether the surgeon or the AI system’s recommendation was to blame.
Key Ethical Concerns:
- Liability: Balancing responsibility between AI and human decision-making.
- Autonomy: The role of human judgment versus AI recommendations.
- Patient Trust: Maintaining trust when AI decisions are overridden.
Benefits:
- More careful integration of AI recommendations into decision-making.
- Clarity on documentation of decisions for legal protection.
- Stronger surgeon-AI collaboration without diminishing human expertise.
4. Data Privacy Breach in AI Surgery
A hospital using AI-assisted surgical tools experienced a data breach, exposing sensitive patient information. This raised ethical concerns about how well AI systems protect patient privacy and the potential risks of storing data within AI networks.
Key Ethical Concerns:
- Data Security: Ensuring patient information is protected in AI systems.
- Transparency: Clear communication with patients about data usage.
- Informed Consent: Patients should know how their data is managed.
Benefits:
- Stronger data protection measures for AI-driven healthcare.
- More stringent consent processes regarding data use.
- Development of secure AI systems to prevent breaches.
5. AI and Organ Transplant Allocation
AI was used to prioritize patients on organ transplant waiting lists. The algorithm was questioned for unfairly disadvantaging older patients, sparking ethical debates about how AI makes life-or-death decisions regarding resource allocation.
Key Ethical Concerns:
- Fairness: Ensuring AI makes decisions based on medical need, not arbitrary factors.
- Accountability: Who is responsible if the AI system’s decision is challenged?
- Patient Consent: Patients must understand how AI affects their place in transplant queues.
Benefits:
- Increased fairness and transparency in AI-driven medical decisions.
- Development of more ethically aligned AI systems.
- Better auditing and review processes for resource allocation decisions.
6. Inaccurate AI Predictions for Post-Surgical Recovery
An AI system incorrectly predicted prolonged recovery times for elderly patients, leading to unnecessary extended hospital stays. This case highlighted the need for continuous improvement in AI systems to avoid biases against certain demographic groups.
Key Ethical Concerns:
- Bias: AI systems failing to account for different patient groups.
- Patient Welfare: How AI-driven decisions affect patient care.
- Accuracy: Ensuring predictions are reliable for all patients.
Benefits:
- More accurate AI predictions through frequent updates.
- Reduced unnecessary medical interventions.
- Greater focus on personalized care to avoid blanket AI predictions.
7. AI in Life-Saving Emergency Surgery
AI provided real-time guidance during an emergency surgery but recommended a high-risk approach. The surgeon followed the AI’s suggestion, but the patient didn’t survive. The ethical issue revolved around the balance between trusting AI in critical moments and surgeon accountability.
Key Ethical Concerns:
- Risk Communication: Ensuring surgeons and patients understand AI recommendations.
- Accountability: Should AI take some responsibility for life-or-death decisions?
- Informed Consent: Did the patient’s family fully understand the risks involved?
Benefits:
- Enhanced guidelines for using AI in high-risk surgeries.
- Surgeons maintaining ultimate decision-making power while using AI insights.
- Increased focus on risk management when AI is involved in critical care.
8. AI in Pediatric Surgery
AI systems were used to assist in pediatric surgeries. Parents raised concerns about whether the AI had been adequately tested for children’s anatomy. This case questioned the ethical implications of using AI systems not designed for specific patient groups.
Key Ethical Concerns:
- Testing and Suitability: Ensuring AI is appropriate for all age groups.
- Parental Consent: Parents must fully understand AI’s role in their child’s surgery.
- Patient Safety: Verifying that AI systems can handle pediatric-specific conditions.
Benefits:
- Improved pediatric AI systems designed specifically for younger patients.
- Better communication with families about AI’s capabilities.
- Development of more tailored AI models to meet diverse patient needs.
9. Surgeon Training with AI Simulation
Surgeons in training used AI to simulate complex surgeries. While the technology improved technical skills, some trainees became overly reliant on the AI’s guidance, sparking concerns that AI could limit the development of critical thinking.
Key Ethical Concerns:
- Over-Reliance on AI: Ensuring surgeons maintain independence in decision-making.
- Training and Autonomy: How AI impacts skill development in surgery.
- Patient Safety: The risk of over-reliance on AI in real-world surgeries.
Benefits:
- More balanced training programs, blending AI with hands-on experience.
- Focus on developing decision-making skills alongside technical training.
- Ethical guidelines ensuring AI doesn’t overshadow human skill-building.
10. AI in Informed Consent for High-Risk Surgeries
In a case where AI played a critical role in recommending a high-risk surgery, the patient argued that they weren’t fully informed about AI’s involvement. This led to legal action, raising questions about the ethical standards of informed consent when AI is heavily relied upon.
Key Ethical Concerns:
- Transparency: Ensuring patients fully understand AI’s role in their treatment.
- Informed Consent: Providing clear, comprehensive information about AI involvement.
- Patient Trust: How to foster trust between AI systems, surgeons, and patients.
Benefits:
- Improved communication regarding AI’s role in surgery.
- Stronger consent processes, with clear explanations of AI’s involvement.
- Enhanced patient trust through better education and transparency about AI systems.
Frequently Asked Questions About Ethical Case Studies in AI Surgery
How is accountability determined when AI is involved in surgery?
Accountability depends on the situation. If the AI system fails or provides incorrect recommendations, the responsibility may be shared between the surgeon, the hospital, and the AI system’s developers. However, surgeons remain responsible for the final decisions made during surgery.
Can AI bias impact surgical outcomes?
Yes, AI bias can lead to disparities in surgical care. If AI systems are trained on non-representative datasets, they may make inaccurate predictions or recommendations for certain patient groups, leading to unequal treatment and potentially worse outcomes.
Are patients informed about AI’s role in their surgery?
Patients should be fully informed about AI’s involvement in their surgery. This includes understanding how AI systems assist the surgeon, what data is being used, and the potential risks associated with using AI in the procedure.
What happens if an AI system fails during surgery?
In the event of an AI malfunction during surgery, the surgeon takes over the procedure. Hospitals should have protocols in place to manage these failures, and the responsibility for the outcome is usually shared between the surgeon and the system’s developer.
Can AI systems replace human surgeons?
No, AI systems are tools designed to assist surgeons, not replace them. AI can provide recommendations and real-time data, but the surgeon remains in control of the operation and makes the final decisions.
What ethical concerns arise from AI’s use in surgery?
Ethical concerns include accountability, bias in decision-making, data privacy, and informed consent. There are also concerns about over-reliance on AI systems, especially when it comes to critical decision-making during surgeries.
Is AI used in all types of surgeries?
AI is not yet used in all surgical procedures. It is more commonly implemented in complex surgeries, robotic-assisted procedures, and areas where large amounts of data need to be processed, such as imaging and diagnostics.
How is AI bias detected and corrected?
Bias in AI systems is typically detected through audits and regular performance reviews. Developers and healthcare institutions need to ensure that the datasets used to train AI are diverse and representative of the entire patient population.
How can surgeons ensure AI recommendations are accurate?
Surgeons must be well-trained in using AI systems and should always combine AI recommendations with their own medical expertise. Transparency in how the AI system arrives at its conclusions also helps surgeons assess the reliability of its recommendations.
Are there regulations governing AI use in surgery?
Yes, various regulatory bodies, such as the FDA in the United States, oversee the development and deployment of AI systems in healthcare. These regulations ensure that AI systems are safe, reliable, and meet the necessary standards before being used in clinical settings.
What role does data privacy play in AI surgery?
Data privacy is crucial in AI-assisted surgeries. Patient data used by AI systems must be securely protected, and patients must give informed consent for their data to be used. Any breaches in data privacy can lead to legal and ethical complications.