Common Symptoms of Vulvitis Explained Briefly
- Intense itching
- Redness and swelling
- Pain and discomfort
- Blisters or ulcers
- Abnormal discharge
Introduction
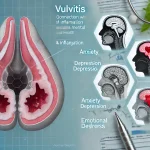
Understanding the symptoms of vulvitis is essential for prompt diagnosis and effective treatment. This inflammation of the vulva can cause significant discomfort and disrupt daily life. We will explore the various symptoms associated with vulvitis, their severity, and the potential underlying causes.
Common Symptoms
Itching
One of the most prevalent symptoms of vulvitis is intense itching. This can be persistent and severe, often leading to scratching, which can further aggravate the condition.
Redness and Swelling
Redness and swelling are common indicators of inflammation. The vulvar area may appear visibly red and swollen, contributing to discomfort and sensitivity.
Pain and Discomfort
Pain and discomfort in the vulvar region are frequent complaints. This can range from mild tenderness to severe pain, impacting daily activities and quality of life.
Blisters and Ulcers
In more severe cases, blisters or ulcers may develop. These can be particularly painful and may indicate an infection or a more serious underlying condition.
Discharge
Abnormal discharge is another symptom associated with vulvitis. The discharge can vary in color, consistency, and odor, often signaling an infection or other issue.
Severity of Symptoms
Mild Symptoms
Mild cases of vulvitis may present with slight itching and redness. These symptoms, while uncomfortable, are usually manageable with basic home care and hygiene practices.
Moderate Symptoms
Moderate vulvitis often involves increased itching, noticeable redness, and swelling. Pain may become more pronounced, requiring medical attention and treatment.
Severe Symptoms
Severe vulvitis can lead to intense pain, significant swelling, blisters, and ulcers. Such cases necessitate immediate medical intervention to prevent complications and promote healing.
Underlying Causes
Infections
Infections, whether bacterial, fungal, or viral, are common culprits behind vulvitis symptoms. Yeast infections and bacterial vaginosis are typical examples.
Allergies and Irritants
Allergic reactions to products such as soaps, detergents, or personal care items can cause vulvitis. Chemical irritants and physical irritants, like tight clothing, also contribute to symptoms.
Hormonal Changes
Hormonal fluctuations, particularly during menopause, can lead to vulvar tissue thinning and increased susceptibility to vulvitis. Hormonal changes impact the severity and frequency of symptoms.
Impact on Daily Life
Sexual Activity
Vulvitis can significantly affect sexual activity, causing pain and discomfort during intercourse. This can impact intimate relationships and overall sexual health.
Urination
Pain during urination is a common complaint, often due to the inflamed tissues. This can make urination uncomfortable and may lead to additional infections if not addressed.
Mobility and Comfort
Severe symptoms can restrict movement, making daily activities challenging. Walking, sitting, and exercising can become painful, affecting overall mobility and comfort.
Diagnosis and Treatment
Medical Consultation
Consulting a healthcare provider is crucial for an accurate diagnosis. Medical history, physical examination, and laboratory tests are essential for identifying the underlying cause.
Treatment Options
Treatment varies depending on the cause and severity of symptoms. Options include medications (antibiotics, antifungals, steroids), home remedies (sitz baths, topical treatments), and lifestyle changes.
Conclusion
Recognizing and understanding the symptoms of vulvitis is vital for seeking timely and appropriate care. By identifying the signs early and consulting healthcare professionals, effective management and relief from vulvitis are achievable. Regular check-ups and maintaining good hygiene practices can help prevent recurrence and improve overall vulvar health.
Top 10 Real-Life Use Cases of AI in Healthcare Management
Predictive Analytics for Patient Outcomes
Technology: Predictive Analytics
Predictive analytics leverages historical data, machine learning algorithms, and statistical techniques to forecast future outcomes. In healthcare, it uses patient data to anticipate health events.
Benefits:
- Early Intervention: Identifies at-risk patients for timely care.
- Improved Outcomes: Reduces hospital readmissions and complications.
- Cost Savings: Minimizes unnecessary treatments and hospital stays.
AI-Powered Diagnostics
Technology: Deep Learning and Computer Vision
AI tools such as deep learning and computer vision analyze medical images (e.g., X-rays, MRIs) to detect diseases like cancer.
Benefits:
- Accuracy: Higher diagnostic accuracy compared to traditional methods.
- Efficiency: Faster analysis and results.
- Accessibility: Enhances diagnostic access in remote areas.
Personalized Treatment Plans
Technology: Machine Learning Algorithms
Machine learning algorithms analyze patient data to create individualized treatment plans based on genetic makeup, lifestyle, and other factors.
Benefits:
- Effectiveness: Increases treatment efficacy.
- Reduced Side Effects: Minimizes adverse reactions.
- Patient Satisfaction: Enhances patient engagement and adherence.
Virtual Health Assistants
Technology: Natural Language Processing (NLP)
Virtual health assistants use NLP to interact with patients, answer queries, and provide medical advice.
Benefits:
- Accessibility: 24/7 availability for patient support.
- Efficiency: Reduces the burden on healthcare staff.
- Engagement: Improves patient compliance with care plans.
Robotic Surgery
Technology: Robotic Systems and AI
Robotic systems, guided by AI, assist surgeons in performing precise and minimally invasive surgeries.
Benefits:
- Precision: Enhances surgical accuracy.
- Recovery: Shortens recovery times.
- Outcomes: Lowers complication rates.
Drug Discovery and Development
Technology: AI and Machine Learning
AI accelerates the drug discovery process by predicting molecule behavior and potential drug candidates.
Benefits:
- Speed: Reduces time to market for new drugs.
- Cost: Decreases research and development costs.
- Innovation: Identifies novel treatment options.
Remote Patient Monitoring
Technology: IoT and Wearable Devices
IoT devices and wearables monitor patients’ vital signs in real-time and transmit data to healthcare providers.
Benefits:
- Continuous Monitoring: Provides constant health updates.
- Early Detection: Identifies health issues early.
- Convenience: Allows patients to stay at home.
Administrative Workflow Automation
Technology: AI and RPA (Robotic Process Automation)
AI and RPA streamline administrative tasks such as scheduling, billing, and claims processing.
Benefits:
- Efficiency: Reduces administrative workload.
- Accuracy: Minimizes human errors.
- Cost Savings: Lowers operational costs.
AI in Emergency Care
Technology: AI Algorithms and Predictive Analytics
AI predicts patient inflow and resource needs in emergency departments, optimizing resource allocation.
Benefits:
- Preparedness: Ensures readiness for emergencies.
- Efficiency: Reduces wait times.
- Patient Care: Improves patient outcomes in critical situations.
AI for Public Health Surveillance
Technology: Big Data and Machine Learning
AI analyzes large datasets to detect and monitor disease outbreaks, guiding public health responses.
Benefits:
- Early Detection: Identifies outbreaks early.
- Response: Facilitates timely public health interventions.
- Resource Allocation: Optimizes use of public health resources.
FAQ on Vulvitis
What is Vulvitis?
Vulvitis is an inflammation of the vulva, which is the external part of the female genitalia. It can be caused by various factors, including infections, irritants, and allergies, leading to symptoms like itching, redness, and swelling.
What are the main symptoms of vulvitis?
The main symptoms include itching, redness, swelling, pain, and sometimes blisters or ulcers. There can also be abnormal discharge and discomfort during urination or sexual intercourse.
How is vulvitis diagnosed?
Diagnosis involves a review of medical history, a physical examination, and laboratory tests such as swabs and cultures to identify infections, as well as blood tests to check for underlying conditions.
What causes vulvitis?
Vulvitis can be caused by bacterial, fungal, or viral infections, chemical irritants such as soaps and detergents, physical irritants like tight clothing, allergies, and hormonal changes.
How can vulvitis be treated?
Treatment options include medications like antibiotics, antifungals, and steroids, as well as home remedies such as sitz baths and topical treatments. Lifestyle changes, such as improved hygiene and avoiding irritants, are also important.
Can vulvitis be prevented?
Prevention involves maintaining proper hygiene, avoiding known irritants, wearing loose-fitting clothing, and having regular medical check-ups to catch potential issues early.
Is vulvitis contagious?
Vulvitis itself is not contagious, but the underlying causes such as infections can be. Identifying and treating the specific cause is important to prevent spreading.
How does vulvitis affect daily life?
Vulvitis can cause significant discomfort and pain, affecting daily activities like walking, sitting, and exercising. It can also impact sexual activity and urination.
Can children get vulvitis?
Yes, children can develop vulvitis, often due to poor hygiene, diaper rash, or irritants. It’s important to maintain good hygiene and consult a pediatrician if symptoms arise.
What should I avoid if I have vulvitis?
Avoid potential irritants such as scented soaps, tight clothing, and products with harsh chemicals. Opt for gentle, fragrance-free personal care items and loose-fitting clothes.
Can vulvitis recur?
Yes, vulvitis can recur, especially if the underlying cause is not fully addressed. Continuous management and preventive measures are crucial to reduce recurrence.
How does menopause affect vulvitis?
Menopause can lead to vulvitis due to hormonal changes, particularly decreased estrogen levels, which cause vulvar tissue thinning and increased susceptibility to irritation and infections.
Are there any home remedies for vulvitis?
Home remedies include sitz baths with warm water, applying cold compresses, and using over-the-counter topical treatments to soothe inflammation and irritation.
What role does diet play in managing vulvitis?
Diet can impact vulvitis, especially if certain foods trigger allergies or irritation. Maintaining a balanced diet and staying hydrated can support overall vulvar health.
When should I see a doctor for vulvitis?
Consult a doctor if symptoms persist despite home care, if you experience severe pain, blisters, or ulcers, or if there are signs of an infection that do not improve with over-the-counter treatments.
Can vulvitis affect my mental health?
Chronic vulvitis can impact mental health, causing stress, anxiety, and depression. Seeking support from healthcare professionals and mental health counselors can help manage these effects.